Study Highlights Semaglutide’s Protective Potential Against Diabetic Retinopathy
New findings presented at the European Association for the Study of Diabetes (EASD) Annual Meeting in Vienna and published in Pharmaceutics suggest that GLP-1 receptor agonists, including semaglutide, may offer significant protective effects against diabetic retinopathy (DR), a leading cause of vision loss in people with diabetes.
GLP-1 Receptor Agonists: Beyond Glucose Control
Semaglutide, a widely used GLP-1 receptor agonist for the treatment of type 2 diabetes and obesity, mimics the GLP-1 hormone by promoting insulin secretion, slowing digestion, suppressing appetite, and increasing satiety. These agents are also being recognized for their potential anti-inflammatory and antioxidant properties.
GLP-1 receptors are present in various tissues throughout the body, including the eye, prompting growing interest in their role beyond glucose regulation.
Diabetic Retinopathy: A Widespread Complication
Diabetic retinopathy, caused by prolonged high blood sugar damaging retinal blood vessels, affects over 90% of individuals with type 1 diabetes and 50–60% of those with type 2 diabetes. The global burden is projected to exceed 191 million cases by 2030, with 56 million at risk of vision-threatening complications.
"This represents a major public health challenge,” noted Dr. Ioanna Anastasiou of the National and Kapodistrian University of Athens, who led the study. “The data highlight the urgency for effective screening, early intervention, and improved therapeutic options."
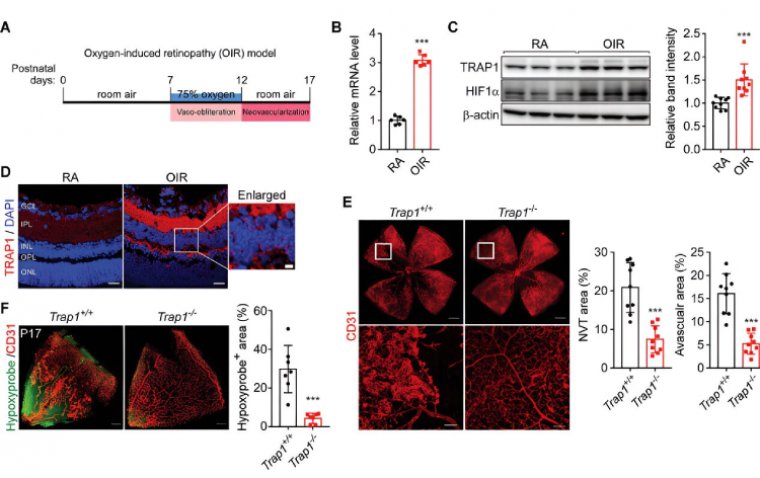
Lab-Based Study Shows Promising Retinal Protection
To assess semaglutide’s effect on retinal health, researchers exposed human retinal endothelial cells to high-glucose, oxidative-stress conditions that simulate a diabetic environment. The cells were treated with varying concentrations of semaglutide for 24 hours and then subjected to viability and stress marker assessments.
Key findings from the in vitro study include:
• Cell survival rates in semaglutide-treated samples were nearly double those of untreated cells.
• Energy stores in treated cells were significantly higher.
• Markers of oxidative stress were dramatically reduced:
• Apoptosis dropped from ~50% in untreated cells to ~10% in treated cells.
• Mitochondrial superoxide production decreased from ~90% to ~10%.
• Advanced glycation end-products (AGEs) accumulation was also substantially reduced.
Furthermore, genes responsible for antioxidant production were notably upregulated in treated cells, suggesting that semaglutide supports both cell protection and repair mechanisms.
Potential to Prevent and Repair Retinal Damage
Dr. Anastasiou emphasized that the study showed no signs of harm from semaglutide to retinal cells. Instead, the data indicates that GLP-1 receptor agonists may be particularly beneficial in the early stages of diabetic retinopathy, possibly even offering restorative effects.
“GLP-1 receptor agonists exerted powerful antioxidant effects which protected retinal cells against diabetes-related damage,” Dr. Anastasiou stated. “Our findings suggest these drugs not only prevent harm but may also help repair existing retinal injury and improve vision.”
Next Steps: Clinical Validation Needed
While the laboratory results are promising, Dr. Anastasiou concluded that clinical trials are essential to confirm these protective effects in patients and to evaluate whether GLP-1 receptor agonists like semaglutide can slow or halt the progression of diabetic retinopathy in real-world settings.
Reference:
Ioanna A. Anastasiou et al, Semaglutide Enhances Cellular Regeneration in Skin and Retinal Cells In Vitro, Pharmaceutics (2025). DOI: 10.3390/pharmaceutics17091115
(1).jpg)