Retinal Thinning Linked to Genetic Risk for Schizophrenia, Study Finds
An international study led by the University of Zurich and the University Hospital of Psychiatry Zurich has revealed a link between retinal thinning and genetic susceptibility to schizophrenia, offering a compelling case for the use of ophthalmic imaging in neuropsychiatric research.
The Retina: A Window into Brain Health
As a direct extension of the central nervous system (CNS), the retina may mirror changes occurring in the brain. In schizophrenia, a disorder characterized by impaired neural information processing, previous studies have already shown reductions in brain gray matter and retinal tissue loss. However, it has remained unclear whether these ocular changes are a cause or consequence of the disease.
Leveraging Large-Scale Genetic and Retinal Data
To investigate this question, researchers utilized the UK Biobank, a biomedical database containing health and genetic information from over 500,000 individuals. The team focused on a large cohort of healthy participants, calculating polygenic risk scores—a measure of inherited risk—for schizophrenia.
“We examined tens of thousands of healthy individuals to determine whether genetic predisposition to schizophrenia correlates with retinal structure,” said Finn Rabe, PhD, first author of the study and postdoctoral researcher at the University of Zurich.
Genetic Risk Linked to Retinal Thinning
Findings, published in Nature Mental Health, confirm that higher genetic risk for schizophrenia is associated with thinner retinas. While the observed effects were small, the scale of the study enabled statistically reliable detection.
Unlike brain imaging, retinal changes can be assessed noninvasively and cost-effectively using optical coherence tomography (OCT)—an ophthalmic technology capable of measuring retinal thickness in minutes. This makes the eye a practical and promising site for monitoring early neurobiological changes.
Implications for Prevention and Clinical Practice
“Our study highlights the potential of using OCT in clinical practice to identify individuals at risk,” Rabe noted. However, he cautioned that large-scale longitudinal studies are required to confirm the clinical utility of these findings for preventive applications.
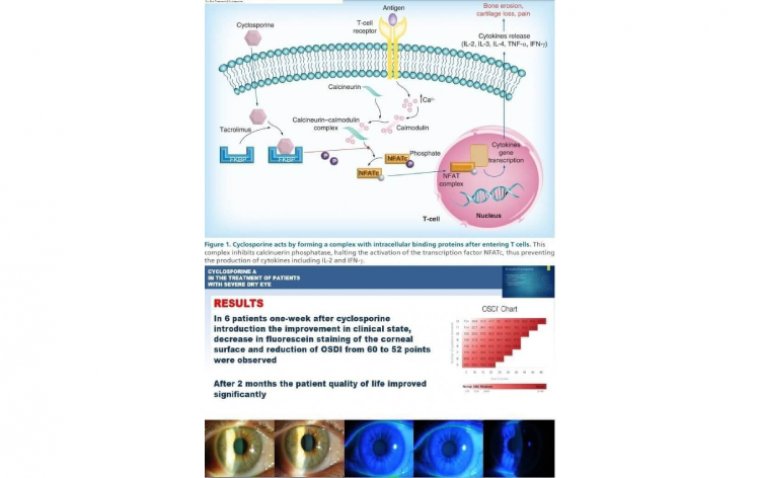
Inflammatory Pathways and Future Therapeutic Directions
Another significant outcome of the study was the identification of genetic variants tied to brain inflammation, which may contribute to retinal structural changes. These findings further support the inflammation hypothesis of schizophrenia, which suggests that neuroinflammation may play a role in disease onset or progression.
“If this hypothesis holds, targeted anti-inflammatory therapies could help mitigate both brain and retinal changes—potentially improving treatment options for patients,” Rabe added.
Reference:
Finn Rabe et al, Genetic susceptibility to schizophrenia through neuroinflammatory pathways associated with retinal thinness, Nature Mental Health (2025). DOI: 10.1038/s44220-025-00414-6
(1).jpg)