NIH Scientists Test Surgical Technique to Enhance Cell Therapy for Dry AMD in Animal Models
Researchers at the National Institutes of Health (NIH) have developed a novel surgical technique that enables the implantation of multiple tissue grafts into the retina—potentially advancing cell-based therapies for dry age-related macular degeneration (AMD). The findings, published in JCI Insight, represent a significant step toward improving regenerative treatments for one of the leading causes of vision loss in older adults.
Addressing the Limitations of Single-Graft Surgery
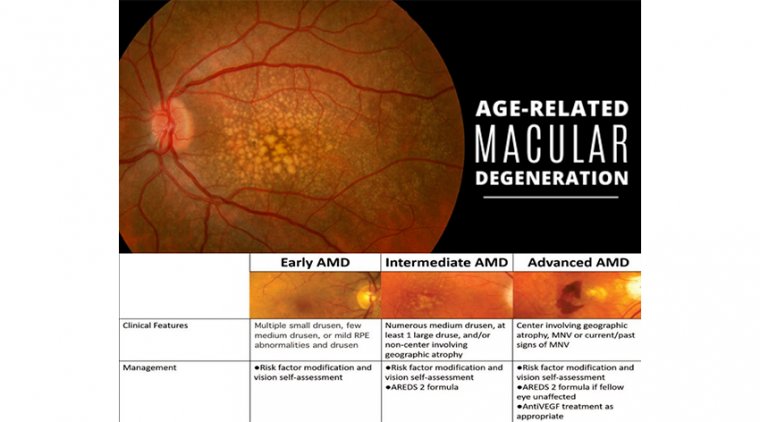
Dry AMD involves the progressive degeneration of retinal pigment epithelial (RPE) cells and photoreceptors, which are essential for capturing light and supporting vision. Scientists have been exploring stem cell-derived RPE grafts as a potential solution to restore function in damaged retinal areas.
Until now, surgical techniques have only allowed the placement of a single tissue graft, restricting both the area that could be treated in clinical settings and the ability to conduct side-by-side graft comparisons in preclinical models. These comparisons are critical for determining the success of graft integration with the retina and the underlying choriocapillaris, the vascular layer that delivers nutrients and oxygen to the retina.
Innovation in Surgical Technique
To overcome these limitations, NIH scientists engineered a custom surgical clamp designed to maintain intraocular pressure, enable back-to-back insertion of two grafts and minimize trauma to surrounding ocular tissues.
Using this approach, researchers successfully implanted two distinct grafts sequentially into the same AMD-like lesion in an animal model, enabling direct comparisons within the same retinal environment.
Experimental Design and Key Observations
In this dual-graft study:
• One graft was composed of RPE cells grown on a biodegradable scaffold, derived from human blood cells converted into stem cells.
• The second graft was composed of the biodegradable scaffold alone, serving as a control.
Following implantation, scientists utilized artificial intelligence (AI) imaging analysis to compare outcomes. The results revealed:
• Photoreceptor survival was significantly higher in areas receiving the RPE graft.
• Photoreceptor loss was more pronounced near the scaffold-only graft.
• Regeneration of the choriocapillaris occurred in the RPE graft area—the first time such regeneration has been confirmed post-implantation.
Implications for Clinical Translation
These findings provide essential insights into the mechanisms by which RPE cell grafts support retinal regeneration, both in terms of photoreceptor preservation and restoration of vascular support via the choriocapillaris.
The study expands on early results from an ongoing NIH-led first-in-human clinical trial, which is currently evaluating the safety and efficacy of patient-derived RPE grafts for the treatment of dry AMD.
Reference:
Rohan Gupta et al, iPSC-RPE patch restores photoreceptors and regenerates choriocapillaris in a pig retinal degeneration model, JCI Insight (2025). DOI: 10.1172/jci.insight.179246
(1).jpg)