Key Indicators of Neuropathic Ocular Pain Identified in Post-LASIK Patients
A study published in the August issue of the American Journal of Ophthalmology has identified critical diagnostic indicators of chronic neuropathic ocular pain (NOP) in patients experiencing chronic dry eye (DE) following laser-assisted in situ keratomileusis (LASIK). The findings offer significant clinical value for ophthalmologists seeking to distinguish between standard dry eye symptoms and neuropathic pain in post-refractive surgery patients.
Comparative Study Highlights Key Differences in Post-LASIK Patients
The prospective cross-sectional comparison study, led by Amanda Vázquez, PhD, from the Institute of Applied Ophthalmobiology at the Universidad de Valladolid in Spain, involved 89 patients divided into three groups: 34 patients with both dry eye and neuropathic ocular pain (NOP-DE), 25 with dry eye only (DE), and 30 asymptomatic LASIK patients serving as controls.
The NOP-DE group showed a significantly greater burden of symptoms and diagnostic markers compared to the DE-only group. Using the Modified Single-Item Dry Eye Questionnaire, the Numerical Rating Scale, and the Wong-Baker Faces Pain Rating Scale, researchers found elevated levels of reported discomfort. This group also showed higher use of ocular lubricants, more frequent pathological outcomes on anxiety and depression scales, and a greater prevalence of central sensitization syndromes.
Objective Corneal Findings Support Neuropathic Diagnosis
Beyond subjective reports, patients in the NOP-DE group demonstrated higher tactile corneal sensitivity after topical anesthesia, suggesting heightened nociceptive response. On in vivo confocal microscopy (IVCM), they exhibited lower corneal nerve density and higher microneuroma density within the sub-basal nerve plexus—both findings consistent with nerve damage or regeneration-related abnormalities.
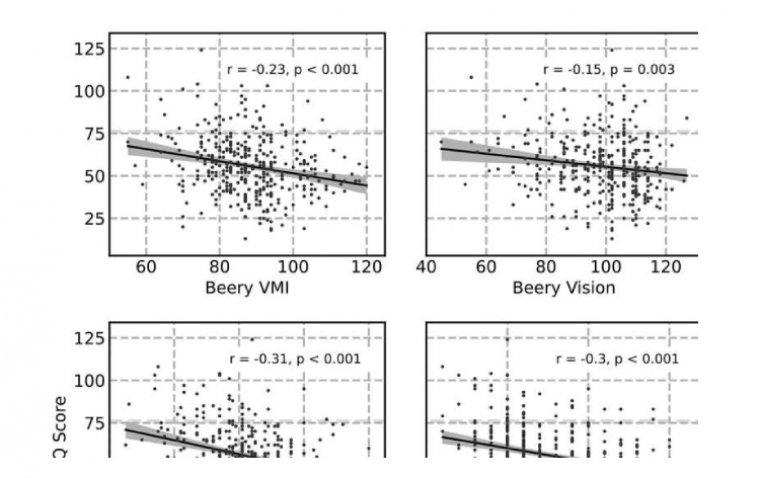
The study found moderate-to-strong correlations between these nerve parameters and the severity of reported symptoms, supporting the use of such objective findings as diagnostic criteria for NOP in post-LASIK patients.
Implications for Diagnosis and Management
The study authors concluded that a combination of reduced nerve density, increased microneuroma formation, and elevated corneal tactile sensitivity after topical anesthesia can serve as diagnostic indicators for identifying neuropathic ocular pain in dry eye patients post-LASIK. These markers may help clinicians differentiate NOP from conventional DE, allowing for more accurate diagnoses and tailored treatment approaches.
Reference:
Amanda Vázquez et al, Corneal Sensory Changes and Nerve Plexus Abnormalities in Chronic Neuropathic Ocular Pain and Dry Eye Postrefractive Surgery, American Journal of Ophthalmology (2025). DOI: 10.1016/j.ajo.2025.04.004
(1).jpg)