Both High and Low HDL Levels Linked to Age-Related Macular Degeneration Risk
A recent study by researchers at the University of California San Diego has revealed a U-shaped relationship between high-density lipoprotein (HDL) levels and the risk of age-related macular degeneration (AMD). Individuals with HDL levels in the middle range showed a lower incidence of AMD, while those with both high and low HDL levels faced an increased risk.
The research also identified specific genetic variants related to HDL metabolism as contributing factors to AMD, shedding new light on the disease’s complex relationship with lipid metabolism.
The Significance of AMD
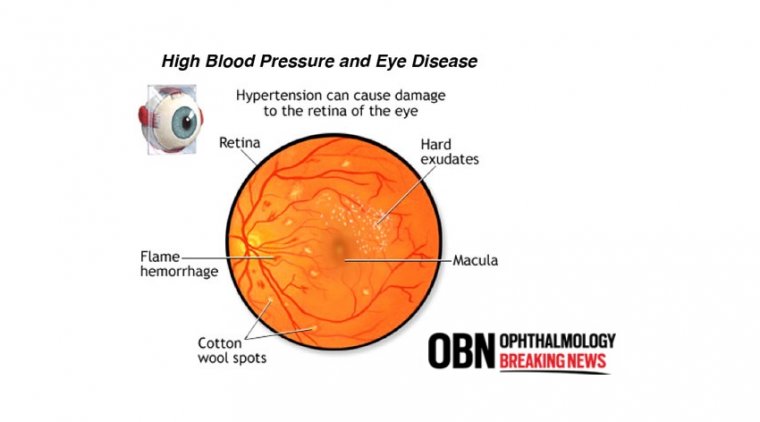
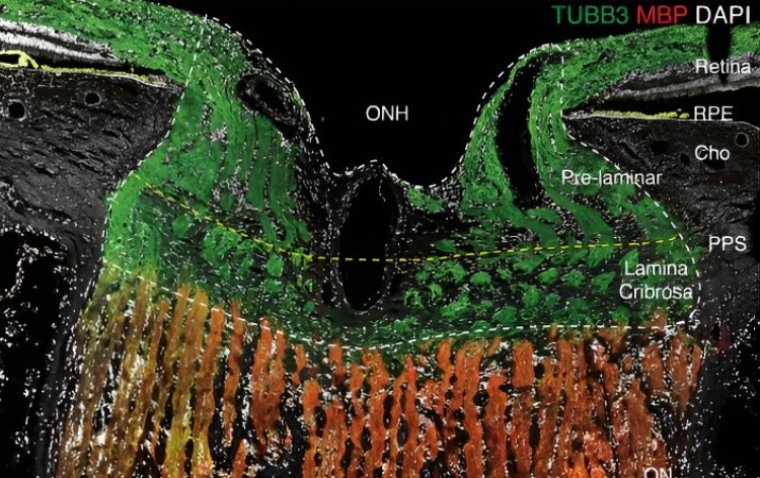
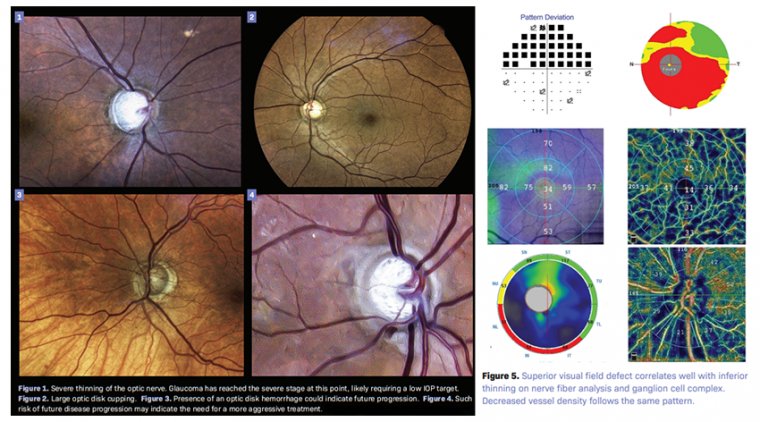
Age-related macular degeneration is the leading cause of legal blindness among older adults in industrialized countries. AMD is characterized by the accumulation of drusen, which are lipoprotein-rich deposits in the retina. The disease’s progression has been linked to dysregulated lipid metabolism, though previous studies have offered conflicting insights into the role of lipids in AMD development.
Study Overview
The findings, published in the journal Ophthalmology, are based on data from the National Institutes of Health's All of Us Research Program. The study titled "High Density Lipoproteins Associate with Age-Related Macular Degeneration in the All of Us Research Program" combined clinical and genetic data to evaluate the impact of lipid metabolism on AMD risk.
Study Design
• Participants: The cross-sectional, retrospective study included 7,356 participants (2,328 AMD patients and 5,028 controls), matched by age, race, and gender.
• Data Analyzed: Clinical data such as smoking status, hyperlipidemia history, and statin use were reviewed alongside laboratory measures of LDL, HDL, and triglycerides. Outliers were excluded.
• Genetic Analysis: Researchers extracted single nucleotide polymorphisms (SNPs) associated with HDL and LDL metabolism using the PLINK toolkit.
Key Findings
1. U-Shaped Association: Multivariable regression analyses demonstrated that both low and high HDL levels were significantly associated with increased AMD risk, forming a U-shaped relationship.
2. Impact of Smoking and Statins: Smoking and statin use were also linked to a higher AMD risk.
3. No Link to LDL or Triglycerides: LDL and triglyceride levels showed no significant correlation with AMD.
4. Genetic Variants and Risk Factors:
• Variants in the ABCA1 and LIPC genes, involved in HDL metabolism, were protective against AMD.
• A novel finding was the association of the LPA gene, linked to lipoprotein(a), as a risk factor for AMD. This is the first study to connect LPA to AMD, suggesting its potential role in drusen formation.
Study Limitations and Future Directions
While the study offers important insights, reliance on retrospective data and diagnostic codes limited the ability to analyze AMD severity. Future research could validate these findings through prospective studies and investigate the potential of lipid-modulating therapies, such as targeting LPA, in preventing or treating AMD.
Conclusion
This study highlights the complex interplay between lipid metabolism and AMD, demonstrating that both high and low HDL levels can increase risk. The findings also open new avenues for understanding genetic risk factors like LPA and their role in AMD pathogenesis, paving the way for innovative approaches to AMD prevention and treatment.
Reference:
Jimmy S. Chen et al, High Density Lipoproteins Associate with Age-Related Macular Degeneration in the All of Us Research Program, Ophthalmology (2025). DOI: 10.1016/j.ophtha.2024.12.039
(1).jpg)