Clearing the Fog: Understanding AMD and How to Protect Your Eyesight
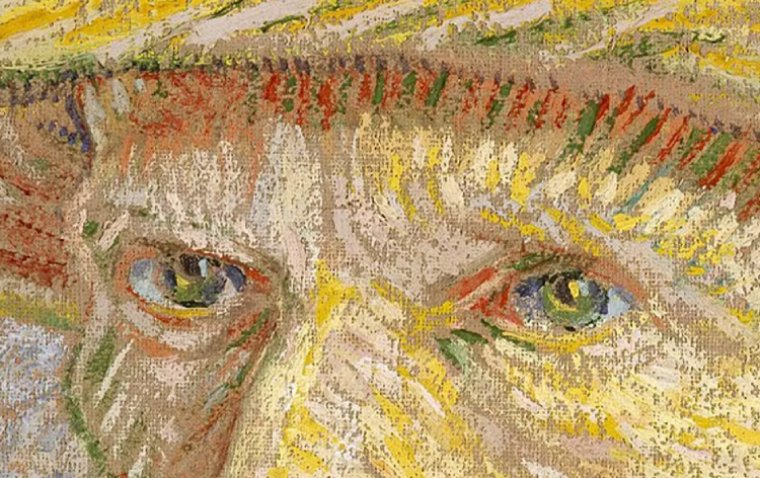
The eyes are often called the windows to the soul, but what happens when those windows become cloudy and blurred? That's the reality for millions suffering from age-related macular degeneration (AMD), which can rob you of your precious eyesight as you age.
But don't despair just yet! In this article, we'll dive deep into the world of AMD, exploring what it is, what causes it, and what you can do to protect yourself from its effects. So sit back, relax, and get ready to learn about this common eye disease and how you can fight back against it. After all, your eyesight is worth fighting for!
What Is Age-Related Macular Degeneration?
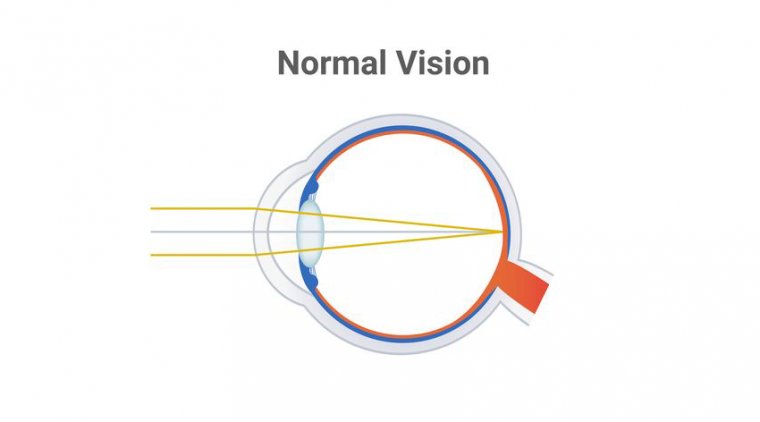
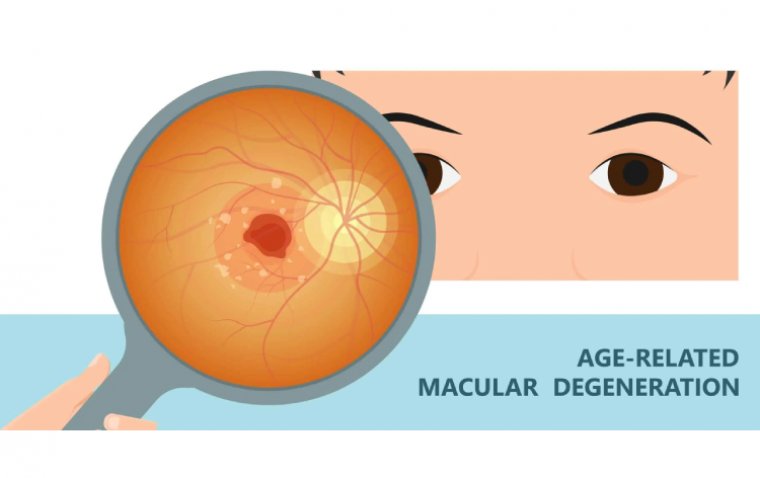
Age-related macular degeneration (AMD) is a common eye disease that affects the macula, the part of the eye responsible for sharp, central vision. It is a leading cause of vision loss in people over 50 and can ultimately lead to blindness if left untreated.
AMD occurs when the macula becomes damaged, either through the buildup of deposits called drusen or through the growth of abnormal blood vessels in the eye. This damage can cause vision to become blurry or distorted, making it difficult to perform everyday tasks like reading, driving, or recognizing faces.
Are There Different Types of Age-Related Macular Degeneration?
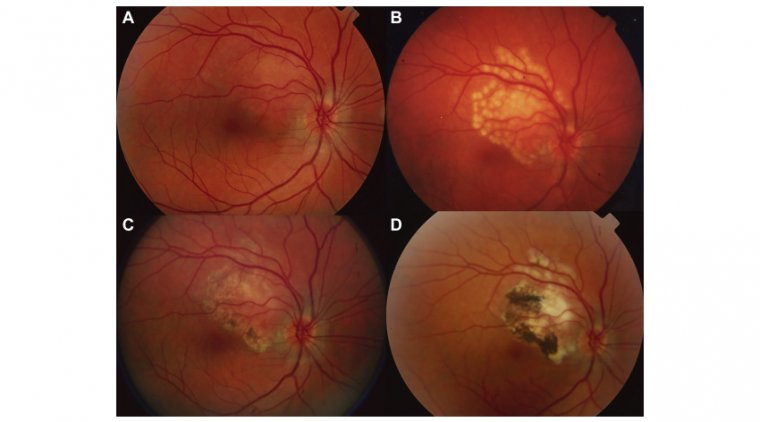
There are two main types of age-related macular degeneration (AMD): dry AMD and wet AMD.
Dry AMD is the most common form of the disease, accounting for about 80% of all cases. It is caused by the gradual breakdown and thinning of the macular tissues, which can lead to the development of small, yellowish deposits called drusen. As the disease progresses, these drusen can grow in size and number, causing further damage to the macula and leading to vision loss.
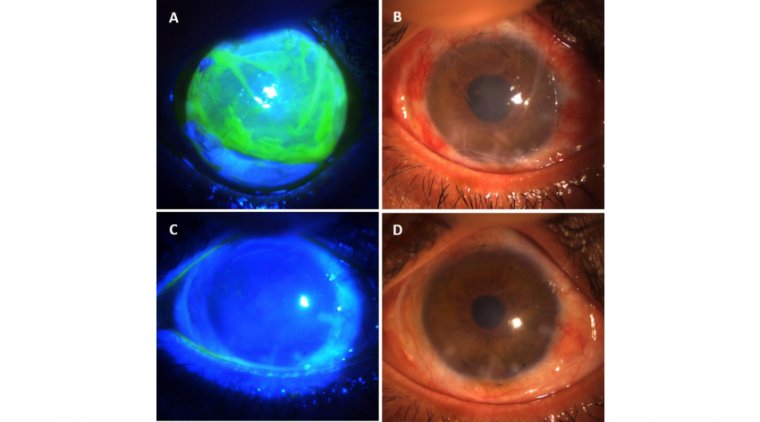
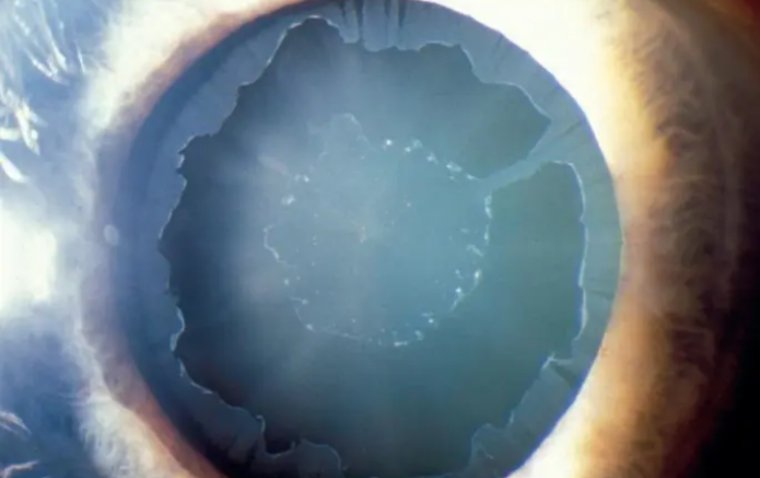
Wet AMD, on the other hand, is less common but more severe. It occurs when abnormal blood vessels grow beneath the macula, which can leak fluid and blood into the eye and cause rapid and severe vision loss. Wet AMD is considered an advanced form of the disease and requires prompt treatment to prevent permanent vision loss.
.jpg)
What Causes Age-Related Macular Degeneration?
The exact cause of age-related macular degeneration (AMD) is not fully understood, but several factors may contribute to its development. These include:
1. Age: As the name suggests, AMD is more common in older adults, with the risk increasing significantly after age 60.
2. Genetics: Studies have shown that certain genetic factors may increase the risk of developing AMD, including genes related to inflammation and the immune system.
3. Smoking: Smoking is a significant risk factor for AMD, as it can damage the blood vessels in the eye and increase inflammation.
4. Poor nutrition: A diet low in fruits, vegetables, and other nutrient-rich foods may increase the risk of developing AMD. In particular, a lack of antioxidants like lutein and zeaxanthin may contribute.
5. Cardiovascular disease: People with conditions like high blood pressure, high cholesterol, and heart disease may be more likely to develop AMD, as these conditions can affect the blood vessels in the eye.
What Are the Symptoms of Age-Related Macular Degeneration?
Age-related macular degeneration (AMD) can cause a variety of symptoms, including:
● Blurred or distorted vision: This is the most common symptom of AMD. You may notice that straight lines appear wavy or objects appear blurry or out of focus.
● Difficulty reading or performing close-up tasks: As AMD affects central vision, you may find it difficult to read small print or perform tasks that require fine detail work, like sewing or knitting.
● Dark or empty spots in your vision: You may notice a dark or empty area in the centre of your vision, making it difficult to see objects directly in front of you.
● Changes in colour perception: Some people with AMD may experience changes in their ability to distinguish colours or notice a decrease in their overall brightness perception.
How Is Age-Related Macular Degeneration Diagnosed?
A comprehensive eye exam usually diagnoses age-related macular degeneration (AMD). During this exam, your eye doctor will perform a series of tests to evaluate the health of your eyes and identify any signs of AMD or other eye conditions.
These tests may include the following:
1. Visual acuity test: This test measures your ability to see clearly at various distances, using an eye chart with progressively smaller letters.
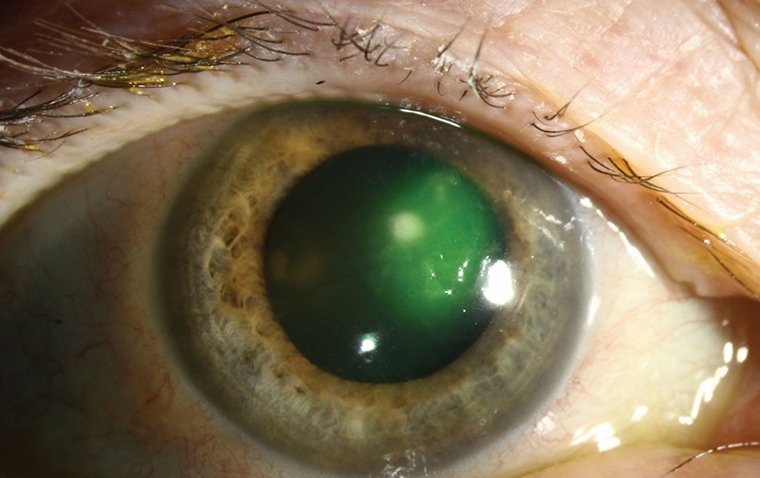
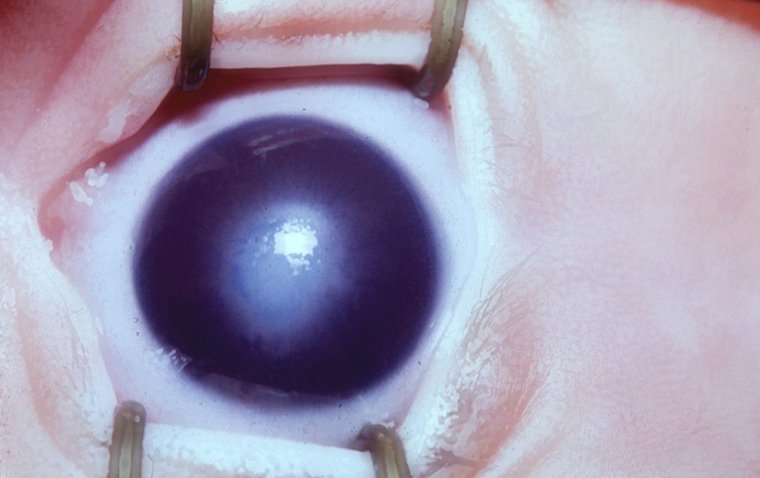
2. Dilated eye exam: Your eye doctor will use unique eye drops to dilate your pupils and examine the back of your eye, including the macula, for signs of AMD.
3. Amsler grid test: This test uses a grid with straight lines to check for distortion or blurriness in your central vision.
4. Optical coherence tomography (OCT): This test uses light waves to create a detailed image of your retina and macula, allowing your eye doctor to detect any abnormalities or damage.
Treatment Options for AMD
The treatment options for age-related macular degeneration (AMD) depend on the type and severity of the disease.
There is currently no cure or specific treatment for dry AMD that can reverse the damage caused by the disease. However, your eye doctor may recommend lifestyle changes to help slow the progression of AMD, such as eating a healthy diet rich in antioxidants, quitting smoking, and taking nutritional supplements like vitamins C, E, and zinc. Regular monitoring of your vision and disease progression is also essential, as advanced cases of dry AMD can sometimes develop into the more severe wet form.
For wet AMD, treatment options include:
1. Anti-VEGF injections: These medications are injected into the eye to block the growth of abnormal blood vessels and prevent further damage to the macula. This is currently the most common treatment for wet AMD.
2. Photodynamic therapy: This treatment involves injecting a light-sensitive drug into the bloodstream, which is then activated by a laser to destroy abnormal blood vessels in the eye.
3. Laser surgery: In some cases, a high-energy laser may destroy abnormal blood vessels in the eye and prevent further damage.
While these treatments can help slow the progression of AMD and preserve your vision, they cannot restore vision that has already been lost. Early detection and prompt treatment are crucial to managing AMD and preserving your eyesight.
Can Age-Related Macular Degeneration Be Prevented?
While there is no guaranteed way to prevent age-related macular degeneration (AMD), there are steps you can take to reduce your risk and slow its progression:
● Eat a healthy diet: A diet rich in fruits, vegetables, and other nutrient-rich foods can help protect your eyesight and reduce your risk of AMD. In particular, foods high in antioxidants like lutein, zeaxanthin, and vitamins C and E may be especially beneficial.
● Exercise regularly: Regular exercise can help reduce your risk of AMD by improving your overall health and reducing inflammation in your body.
● Quit smoking: Smoking is a significant risk factor for AMD, so quitting smoking can significantly reduce your risk of developing the disease.
● Protect your eyes from UV rays: Exposure to UV rays can damage your eyes and increase your risk of AMD. Wearing sunglasses with 100% UV protection and a wide-brimmed hat can help protect your eyes from harmful rays.
● Control your blood pressure and cholesterol: High blood pressure and cholesterol can increase your risk of AMD, so working with your doctor to manage these conditions are essential.
● Get regular eye exams: Regular eye exams can help detect AMD and other eye conditions early when they are most treatable.
In conclusion, age-related macular degeneration (AMD) is a severe eye disease that can significantly impact your vision and quality of life. While there is no guaranteed way to prevent AMD, you can take steps to reduce your risk and slow its progression. By eating a healthy diet, exercising regularly, quitting smoking, protecting your eyes from UV rays, and getting regular eye exams, you can help protect your eyesight and maintain your independence for years. So take care of your eyes and prioritize your vision - your future self will thank you!
Author: Dr. Muhammad Saad, Resident Ophthalmologist at Al-Shifa Trust Eye Hospital in Rawalpindi, Pakistan
(1).jpg)