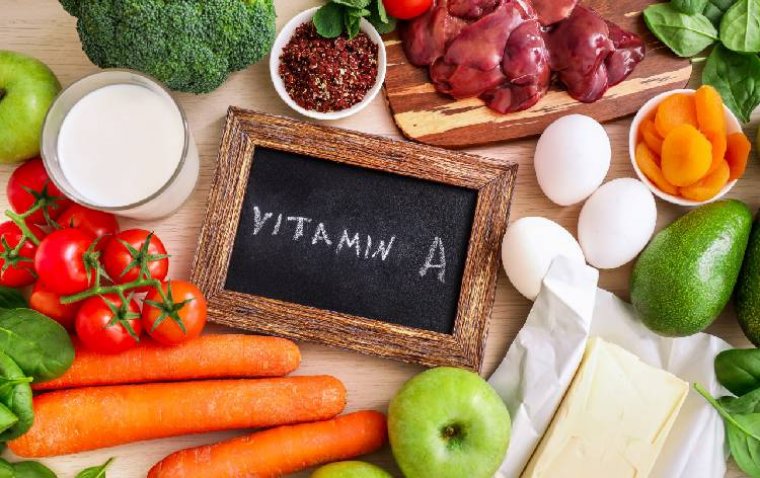
Vitamin A & The Ocular Surface
Vitamin A deficiency remains an important cause of ocular morbidity among patients with chronic liver disease and lipid malabsorption, and is a major cause of blindness in developing countries.
Early ocular surface changes include keratinization of the conjunctiva and development of superficial punctate keratopathy. More severe deficiency results in corneal keratinization, ulceration, and necrosis.
Vitamin A is necessary for normal differentiation of nonsquamous epithelium; keratinization is a direct consequence of its deficiency.
Exposure exacerbates the process and surface phenomena, especially localized drying from loss of mucus-secreting goblet cells, reduced aqueous tear production, and irregularities of the keratinized surface may all contribute to stromal melting, which can occur in the absence of inflammatory infiltration or bacterial invasion.
Surface abnormalities respond rapidly to systemic vitamin A. Significantly, corneal changes disappear long before the reappearance of goblet cells. Inflammation sometimes masks or reverses the xerotic process.
The World Health Organization lists vitamin A deficiency as one of the most important causes of preventable childhood blindness.
Dysfunction of corneal and conjunctival epithelial cell differentiation governed by vitamin A results in graded abnormalities in the ocular surface ranging from punctate epithelial erosions to corneal perforation.
It can be initially misdiagnosed since the signs are easily mistaken for epithelial erosions seen in keratoconjunctivitis sicca or exposure keratopathy.
Without treating the underlying vitamin A deficiency, these ocular surface conditions are progressive and refractory to lubricating therapy or even surgical intervention.
Vitamin A is a vital, fat-soluble nutrient found in various foods including dairy products, meat, and certain types of fish (National Institutes of Health, 2021).
It is absorbed in the intestinal lumen and converted into natural retinoid derivatives such as retinol, retinoic acid, and retinaldehyde (Samarawickrama et al, 2014). Vitamin A acts positively on the immune and reproductive systems and, notably, on the visual system (NIH, 2021).
It aids numerous visual functions including post-traumatic corneal healing, conjunctival goblet cell renewal (Samarawickrama et al, 2014), and rhodopsin production in the photoreceptors to maintain vision (NIH, 2021).
A vitamin deficiency may lead to serious systemic and ocular complications such as respiratory infections, gastrointestinal problems, xerophthalmia, nyctalopia, and corneal ulceration (Wu, 2015).
Several retinol derivatives are used in medicine and in cosmetic applications in topical or systemic formulations. This article discusses the effects of vitamin A and its derivatives on the ocular surface, particularly with respect to the tear film and the meibomian glands.
Impact of Systemic Vitamin A on the Ocular Surface Isotretinoin (13-cis retinoic acid [RA]) is an oral medication used to treat advanced forms of acne by acting on sebaceous glands of the skin, with the goal of decreasing inflammation and sebum production (Tanriverdi et al, 2021).
In vitro studies have shown that 13-cis RA provokes cellular changes and significantly alters gene expression in the meibomian glands (P < 0.05), causing increased cellular destruction and necrosis (Ding et al, 2013).
This can lead to meibomian gland atrophy and to altered secretions, which are key factors in dry eye disease (Düzgün et al, 2020). 2021; Mathers et al, 1991) and may affect the ocular surface.
Furthermore, increased osmolarity of the tears, blepharitis, and contact lens intolerance have been reported in conjunction with oral use of 13-cis RA (Tanriverdi et al, 2021).
Impact of Topical Vitamin A on the Ocular Surface
Although the ocular side effects of systemic vitamin A derivatives are well established in the literature, there is a paucity of information on its topical use. Because of its anti-aging effect (Kafi et al, 2007), 13-cis RA is a common ingredient in cosmetics (Ding et al, 2013).
While topical creams are known to exhibit minimal absorption through the skin, a month-long facial application of a retinoid/antibiotic cream resulted in a significant (P < 0.001) increase in symptoms (measured using the Ocular Surface Disease Index questionnaire) and tear osmolarity as well as a decrease in tear stability (Bayhan et al, 2016).
Limitations of the study included its short duration (one month) and the lack of meibomian gland imaging and of assessment of ocular symptoms and signs post-treatment. Longer studies are warranted to ascertain whether these effects persist.
This leads to lower lipid production and to increased tear film evaporation. The meibomian glands seem to be affected uniformly when using 13-cis RA (Mathers et al, 1991).
This finding can be used to differentiate its effects from other causes of meibomian gland dysfunction, which result in nonsymmetrical atrophy of the glands (Mathers et al, 1991).
While the function of the lacrimal gland remains intact, systemic absorption of oral 13-cis RA may be found in the tears through its secretions (Tanriverdi et al, 2021; Mathers et al, 1991) and may affect the ocular surface.
Furthermore, increased osmolarity of the tears, blepharitis, and contact lens intolerance have been reported in conjunction with oral use of 13-cis RA (Tanriverdi et al, 2021).
(1).jpg)