Sleep Apnea Linked to Increased Risk of Wet Age-Related Macular Degeneration
A new study by the Center for Eye Research Australia (CERA) has identified a potential link between obstructive sleep apnea (OSA) and wet age-related macular degeneration (AMD). Published in Clinical and Experimental Ophthalmology, the findings suggest that low oxygen levels in the blood overnight—a common sign of OSA—could be a modifiable risk factor for late-stage AMD.
Study Overview: Investigating the Sleep-AMD Connection
The research was conducted by University of Melbourne Master’s student Attiqa Chaudhary alongside CERA’s Macular Research unit, led by Professor Robyn Guymer AM. The team collaborated with sleep disorder expert Professor Matthew Naughton from Monash University to analyze the results.
The study involved 225 participants over the age of 50, all at different stages of AMD. Over three nights, researchers measured their oxygen levels using a home-based finger oximeter to assess the severity of their OSA.
Findings: Moderate-to-Severe OSA Increases Wet AMD Risk
The results revealed that participants with moderate-to-severe OSA, characterized by lower oxygen levels overnight, had a higher risk of developing wet AMD compared to those without OSA.
Study co-supervisor Dr. Carla Abbott emphasized the significance of these findings for clinicians.
"Like AMD, sleep apnea mainly affects people over the age of 50, and many people don’t realize they have it," Dr. Abbott stated.
She further suggested that screening for sleep apnea in high-risk AMD patients could be beneficial, as treating OSA might reduce the risk of progressing to wet AMD.
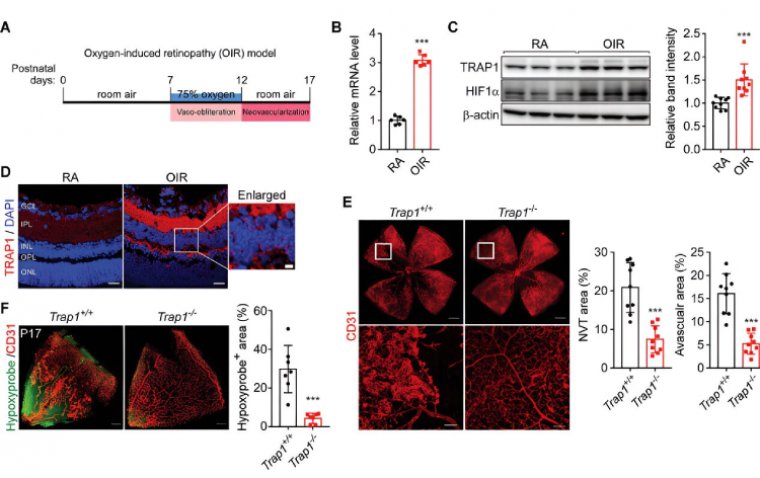
The Role of Nocturnal Hypoxia in Retinal Health
Nocturnal hypoxia, a drop in oxygen levels during sleep, is a common consequence of OSA. This condition occurs when a person’s airway becomes blocked or narrowed, restricting their oxygen intake.
Dr. Abbott explained that the retina is highly active at night, requiring significant amounts of energy to recover from daily exposure to light. This high metabolic demand may make the retina particularly sensitive to even small reductions in oxygen levels.
Can Treating Sleep Apnea Help Prevent AMD?
Many OSA patients use a CPAP (Continuous Positive Airway Pressure) device, which helps maintain an open airway and improves oxygen intake during sleep.
According to Dr. Abbott, untreated OSA could pose a long-term risk by contributing to poor sleep quality and chronic nocturnal hypoxia, potentially increasing the likelihood of developing wet AMD.
While smoking, diet, age, and genetics are already established AMD risk factors, this study raises the possibility that OSA may also play a role.
Next Steps: Further Research to Confirm the Link
The CERA team plans to conduct larger studies to further investigate the connection between sleep apnea and AMD. If the link is validated, future research will explore whether treating OSA can help slow or prevent AMD progression.
This work is part of the Synergy High Risk AMD Study, which aims to uncover underlying causes of AMD and identify new ways to protect vision.
Reference:
Attiqa Chaudhary et al, Nocturnal hypoxia and age‐related macular degeneration, Clinical & Experimental Ophthalmology (2024). DOI: 10.1111/ceo.14428
(1).jpg)