The Cataract Journey & Role Of Medical Staff – Patient Care
Cataract surgery is the most frequently performed operative procedure worldwide, typically concludes with the implantation of an artificial intraocular lens (IOL) to correct aphakia (absence of the crystalline lens).
The surgery—which involves removing the eye’s clouded lens and replacing it with a clear synthetic version—once required several days in the hospital and a long recovery period.
Cataract surgery is performed under local anesthesia on an outpatient basis, and people are back to their normal lives within days. The success rate is high, and the rate of vision-threatening complications is relatively low.
For people with cataracts, the decision whether to have surgery may be easy to make. However, two additional decisions might be more difficult: when to have surgery and what type of lens implant to get.
Cataract surgery is a rite of passage for most people in their 60s and 70s. To surgeons, it’s an efficient, time-tested procedure with predictably excellent outcomes; for patients, however, the journey to the OR can be worrisome.
Questions abound, as they look for guidance and reassurance from everyone they encounter along the way. As surgeons, we have limited time to spend with each patient, which makes the role of our staff so incredibly important.
Most patients, unless they were referred to us specifically for a cataract evaluation, don’t even know they have a visually significant cataract. They come to us because they have blurred vision or because they’re unable to see clearly when driving at night.
When they learn they have a cataract — and that surgery is required to treat it — they become nervous and fearful. All they hear is, “surgery on my eye.” At every touchpoint along the way, from diagnostic testing to postoperative care, our staff members are educating, supporting, and encouraging patients.
THE JOURNEY BEGINS WITH KEY TESTS
Patients referred to us by a co-managing optometrist for a cataract consult will have completed our dry eye questionnaire and will have undergone tear osmolarity, MMP-9 (InflammaDry; Quidel), meibography, and OCT of the macula.
While performing these tests, our screening technicians explain to patients what the tests are and how they will help the surgeon achieve more accurate outcomes. We assess contrast sensitivity (CSV-1000; Vector Vision) for all patients, starting at age 50, to demonstrate day and night driving vision.
It’s not uncommon for a patient to have 20/25 visual acuity on the Snellen chart, but report serious difficulty while driving at night.
We’ve seen a patient’s visual acuity drop from 20/25 to 20/70 during simulated night driving. When we can say, “Wow! No wonder you’re having trouble driving at night,” the patient is relieved to learn that there’s something concrete going on.
Importantly, we always follow that pronouncement with, “And we have a solution for you.” We are not just telling patients they have cataracts; we are immediately informing them that we can safely remove cataracts, improve their vision, and, possibly, reduce their dependence on eyeglasses. This is a cornerstone of our cataract patient education.
OFFER INFORMATION AND REASSURANCE
While a patient’s pupils are dilating, we show a brief educational video that explains in lay terms what a cataract is, how we treat it and the vision correction options.
After the video, we enter the room with a scribe, review the patient’s test results, and confirm the presence of visually significant cataracts.
We explain that we will email some additional videos about implants and astigmatism correction options for the patient to watch before the next appointment. After we leave the room, our scribe reinforces what we just discussed, answers any additional questions, and offers reassurance and suggestions for the patient to consider for the next appointment.
The conversation will likely touch on the following, often in these exact words:
- “Cataract surgery is safe.”
- “We have performed thousands of cataract surgeries, and our patients are very happy.”
- “After watching the educational videos, write down any questions you may have and bring them to your next appointment
- “After we take the various eye measurements required for surgery, we will decide together the type of implant that best suits your needs.”
Our approach is designed to empower patients and provide the tools for them to become educated about implant options. The scribe then introduces the patient to our surgical coordinator, who describes our process going forward, including preoperative and postoperative care.
At this time, the preoperative visit is scheduled, the surgery date is selected, and all postoperative appointments are set, giving the patient time to arrange for transportation.
PRESURGICAL DATA INFORMS DECISIONS
When patients return for their presurgical measurements (after undergoing treatment for an ocular surface disease, if necessary), our technicians are once again front and center, providing critical data to help ensure the best possible outcomes.
Our biometrist obtains all measurements using various machines — IOLMaster 700 (Zeiss), OPD-Scan III (Nidek), Cassini corneal topographer (optics) — for biometry, keratometry, and topography, all while explaining to the patient what each machine and test tells us about their vision and ocular health.
Now, perhaps for the first time, the patient may be hearing the word “astigmatism,” prompting the technician to explain what that means and to reassure the patient that it can be corrected.
When we see the patient review all of the presurgical data, we are confident he or she already has some basic information that we can build upon.
Patients can feel overwhelmed by the sheer volume of information they’re receiving. Therefore, we tailor our discussions to each patient and describe only the options that are suitable for that patient, including steps we take to ease the postoperative experience, such as administering an extended-release steroid intraoperatively to reduce the number of eye drops needed postoperatively.
In our practice, we don’t use the word “premium” to describe IOLs. Instead, we discuss “advanced technology” lenses, which is scientific, rather than subjective, terminology. After considering the pros and cons of each option, the patient and we decide together what will work best.
Patients are much more engaged in their medical decisions than they were even a decade ago when they were more inclined to accept a doctor’s word as final.
Today, patients often arrive in our office with some knowledge, and they want to participate in selecting the type of surgery, the type of implant, and so on. These decisions are much more collaborative than in the past.
THOUGHTFUL POSTSURGICAL FOLLOW-UP
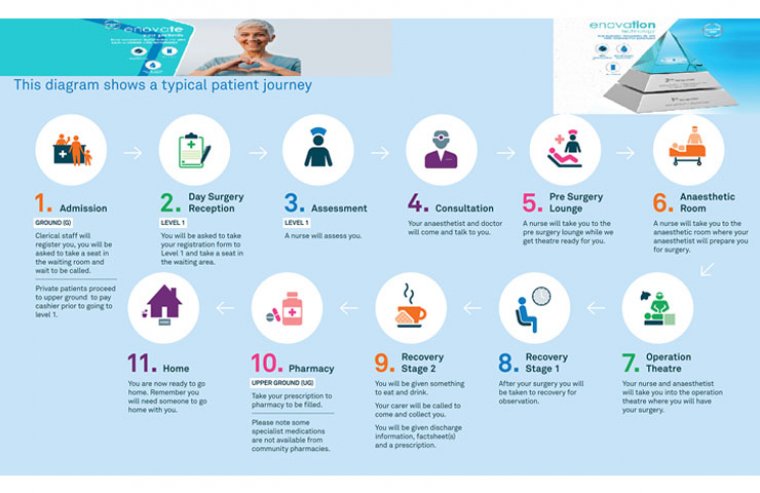
On surgery days, we work with the surgery center personnel. Although they are not members of our staff, they are true professionals, keeping patients informed and reassured as they focus on the tasks required for surgery.
Postoperative care is aimed to prevent infection, control inflammation, and minimize ocular pain. Traditionally, surgeons have prescribed antibiotics, steroids, and NSAID eye drops to be administered by patients at home after cataract surgery.
This regimen, which can span 6 weeks or more, involves hundreds of drops and can be difficult to follow, particularly for patients with poor dexterity or memory problems.
HELPING PATIENTS MANAGE TOPICAL MEDICATIONS
We use many “dropless” components during cataract surgery, including extended-release intracameral or intracanalicular steroids and combination medications, but some topical drops still may be required for certain patients.
For example, we may prescribe an antibiotic, a steroid, an NSAID, or all three medications to minimize the risk of infection or inflammation for patients with certain preexisting comorbidities. If we perform a limbal relaxing incision (LRI) to treat astigmatism, we prescribe an antibiotic eye drop.
Although we may be minimizing the use of topical drops, we’re still not 100% dropless. Our technicians play a key role in teaching cataract patients the pre-and postoperative drop regimen. They explain the reason for each medication, how to safely instill the drops, and how often they should be used.
They instruct patients to wait at least 10 minutes between instilling drops and why that’s important. We give patients instruction sheets detailing their regimen, but the one-on-one training and staff demonstrations are invaluable for reinforcing this critical step toward a successful outcome.
On the same day after the surgery, a member of our staff follows up by phone with all patients to ask how they’re doing and if they or their caregivers have any questions. It’s important to remind patients what to expect after surgery and what their responsibilities and precautions are.
The staff member may repeat some of the usual precautions: no swimming or using a hot tub; no putting pressure on the operated eye while dabbing after instilling drops, no mascara for a month to avoid rubbing the eye to remove it; remember to wear the eye shield while sleeping; and be sure to wash your hands before instilling your eye drops.
Although these little checks are second nature to eyecare professionals, they’re not necessarily intuitive to patients. We find that patients still have questions on the day of surgery after they go home. A brief explanation goes a long way to ease a patient’s anxiety.
CONSISTENT MESSAGING
As patients make their way through our practice on the way to cataract-free vision — the vision they will have for the rest of their lives — we strive to deliver consistent information in easy-to-understand language.
Whether we educate patients verbally, either in the office or by phone, or visually through videos and printed material, we know that clinical terminology or confusing data can hamper their ability to make a crucial decision.
To help us maintain a high level of knowledge and consistent messaging, we hold staff training sessions every week. We include our front desk receptionists, our billing associates, and our ophthalmic assistants — anyone who is likely to interact with patients.
ADVANCED TRAINING
Typically, it’s the responsibility of the practice and the surgeon to teach clinical staff about the different intraoperative procedures and new drug deliveries. Staff must know these topics well, so they can accurately discuss them with patients in terms they will understand in a caring and supportive manner.
In terms of post-cataract surgery care, for example, the new sustained-release intracameral and intracanalicular steroids are leading to a shift away from patient-administered topical drops at home.
Not only are these drug delivery systems helping to relieve patients of the hassle of instilling multiple drops per day for extended periods, but they also take compliance out of the hands of patients.
Our staff needs to understand these new options so they can explain them to patients. We encourage our technicians to become certified ophthalmic assistants. Also, we include material from the COA home study book in our own training sessions. There’s always learning going on in our practice.
WELL-EDUCATED STAFF INSPIRES PATIENTS’ CONFIDENCE
Our staff members need to be well-educated, so they can speak confidently and explain in a positive, non-threatening way what a cataract is, the steps involved in removing it, review postoperative care, and emphasize the benefits patients can derive from cataract surgery.
(1).jpg)