Exploring Ischemic Optic Neuropathy and its Impact on Vision
What Is Ischemic Optic Neuropathy?
Ischemic Optic Neuropathy (ION) refers to a type of vision loss that occurs due to reduced blood flow to the optic nerve, the critical structure responsible for transmitting visual signals from the eyes to the brain. In essence, the optic nerve doesn't receive enough oxygen-rich blood, leading to damage and subsequently compromised visual function.
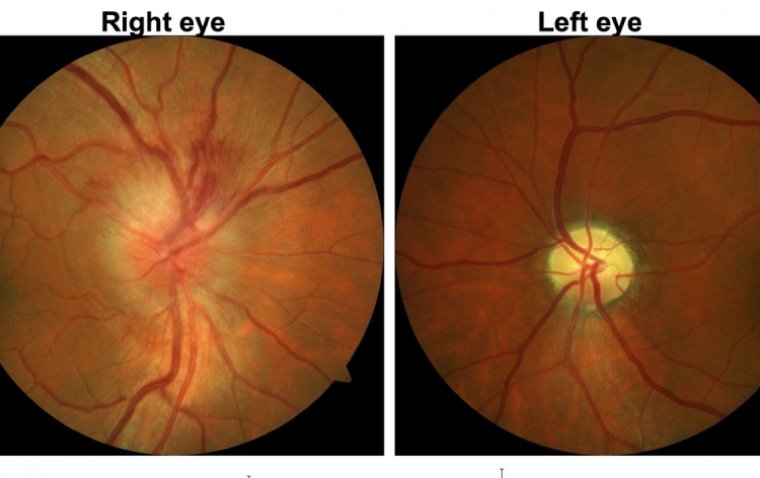
There are two main forms of ION: Anterior Ischemic Optic Neuropathy (AION) and Posterior Ischemic Optic Neuropathy (PION). AION, the more common of the two, affects the front (anterior) part of the optic nerve, usually visible upon examination of the retina. In contrast, PION impacts the posterior section of the optic nerve, which is not visible through a standard eye exam.
Several factors can lead to ION, ranging from systemic conditions like hypertension and diabetes to specific ocular diseases. Recognizing the signs and understanding its causes is crucial for timely intervention and optimal management.
Main Types of Ischemic Optic Neuropathy
1. Anterior Ischemic Optic Neuropathy
Anterior Ischemic Optic Neuropathy (AION) is a form of Ischemic Optic Neuropathy that primarily affects the anterior or front portion of the optic nerve. This segment of the nerve is located near the retina's surface, making its effects directly observable during a fundoscopic examination.
AION is primarily categorized into two subtypes:
● Non-Arteritic Anterior Ischemic Optic Neuropathy (NAION): The most common type, NAION, occurs spontaneously due to transient reduction of blood flow, often during sleep. Risk factors for NAION include hypertension, diabetes, certain medications, and specific structural eye characteristics.
● Arteritic Anterior Ischemic Optic Neuropathy (AAION): Less common but more severe, AAION results from inflammation of the arteries supplying the optic nerve, commonly linked to a condition called Giant Cell Arteritis. Immediate medical intervention is required to prevent further vision loss or involvement of the other eye.
2. Posterior Ischemic Optic Neuropathy
Posterior Ischemic Optic Neuropathy (PION) is a less common form of Ischemic Optic Neuropathy when compared to its anterior counterpart. It involves the posterior portion of the optic nerve, which is situated behind the eye and isn't directly visible during a routine eye examination.
Unlike AION, PION does not show evident optic disc swelling when examined with an ophthalmoscope, especially in its early stages. This makes its diagnosis a bit more challenging, relying on a combination of clinical history, vision examination, and sometimes advanced imaging techniques to visualize the posterior optic nerve.
The causes of PION include:
● Vascular: Reduced blood flow to the posterior optic nerve due to various factors, such as hypotension, blood loss, or shock.
● Surgical: PION has been documented after certain surgeries, especially spine or cardiac surgeries, where there might have been significant blood loss or periods of decreased blood pressure.
● Inflammatory or Infectious: Rarely, inflammation or infections can lead to PION.
● Others: Certain conditions and medications can increase the risk of PION, but they are less commonly implicated than the above causes.
Ischemic Optic Neuropathy Causes and Risk Factors
Ischemic Optic Neuropathy (ION) is primarily classified into two main categories based on its causes: arteritic and non-arteritic. Each has its own distinct set of risk factors and underlying mechanisms, making a comprehensive understanding essential for diagnosis and management.
Arteritic vs. Non-Arteritic Causes
1. Arteritic ION (AION): This form is associated with inflammation of the arteries, most commonly due to a condition called giant cell arteritis (GCA). GCA leads to inflammation of medium and large arteries, especially those supplying the optic nerve, causing a sudden and profound vision loss. Key symptoms also include headache, scalp tenderness, and jaw claudication. Immediate diagnosis and treatment with corticosteroids are essential to prevent vision loss in the other eye.
2. Non-Arteritic ION (NAION): More common than AION, NAION is not due to inflammation but instead results from factors that compromise blood flow to the optic nerve. Its presentation is less severe than AION but can still lead to significant vision impairment.
Role of Vascular Disorders and Systemic Diseases
Vascular disorders are at the core of ION. Reduced blood flow, whether due to inflammation (as in AION) or other circulatory problems (as in NAION), can lead to optic nerve damage. Systemic conditions, such as diabetes, can compromise blood vessels' integrity, making them more susceptible to blockages. Similarly, conditions like sleep apnea can cause fluctuations in oxygen levels, potentially affecting optic nerve blood flow.
Signs and Symptoms of Ischemic Optic Neuropathy
Ischemic Optic Neuropathy (ION) is characterized by a sudden or gradual compromise of the optic nerve's blood supply, leading to a range of visual disturbances. Recognizing the signs and symptoms early is crucial, as the condition can significantly impact one's quality of life.
1. Visual Disturbances and Vision Loss
● Sudden Vision Loss: One of the hallmark symptoms of ION, especially in its non-arteritic form (NAION), is a sudden decrease in vision. Affected individuals may wake up to find that their vision in one eye has notably diminished.
● Visual Field Deficits: People with ION often experience specific patterns of vision loss. Altitudinal field defects are common, where either the upper or lower half of the visual field is lost. Central vision, however, may still be preserved in some cases.
● Blurred or Dim Vision: Alongside specific visual field losses, generalized blurring or dimness of vision may be experienced, making it difficult to see fine details.
● Color Vision Impairment: The perception of colors may become dulled or altered, making it difficult to distinguish between shades.
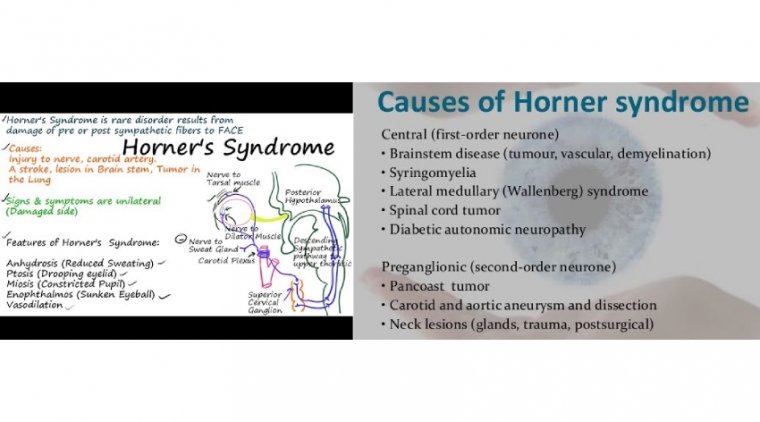
● Pupillary Abnormalities: The affected eye's pupil might react abnormally or slower to light due to impaired optic nerve function.
2. Sudden vs. Gradual Onset
● Sudden Onset: Typically seen in Non-Arteritic ION (NAION), the symptoms manifest abruptly. Individuals might go to bed with normal vision and then wake up with noticeable visual impairment in one eye. This sudden onset can be alarming, necessitating immediate medical attention.
● Gradual Onset: Arteritic ION (AION), often linked with giant cell arteritis, might present with more gradual symptoms. However, the progression can still be relatively rapid over days. Symptoms such as temporal headache, jaw claudication, or scalp tenderness may accompany the vision loss, indicating an underlying inflammatory process.

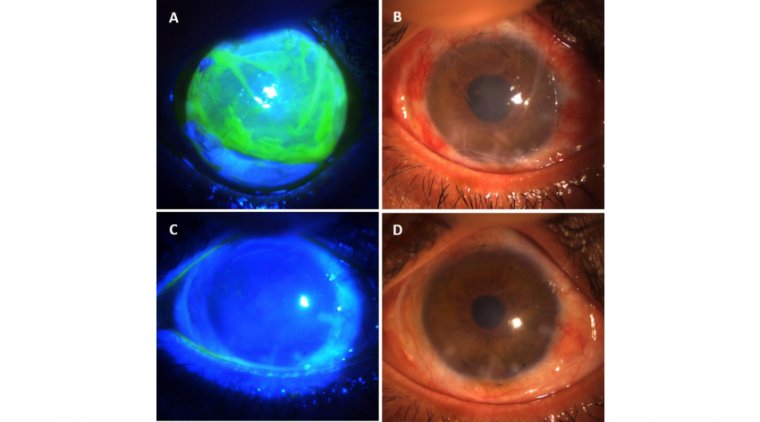
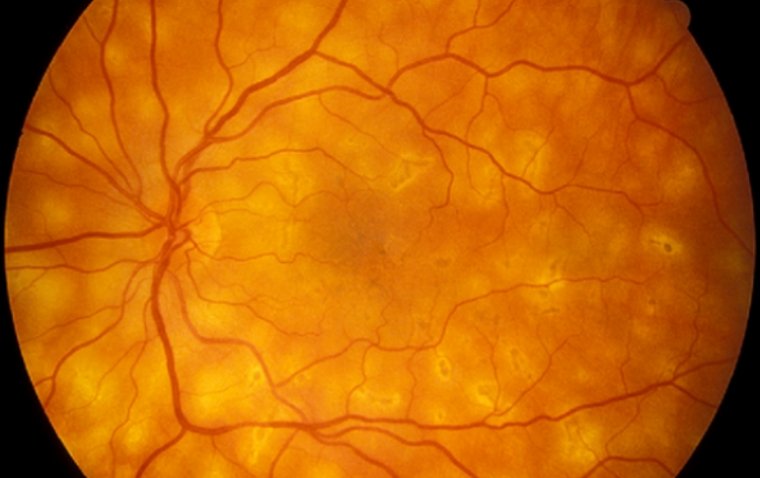
Credit: Review of Ophthalmology
Diagnosing Ischemic Optic Neuropathy
Ischemic Optic Neuropathy (ION) is a serious ocular condition that results from a compromised blood supply to the optic nerve. Timely and accurate diagnosis is critical to prevent further damage and to manage any underlying causes. Let's explore the diagnostic procedures used to identify ION.
Comprehensive Examination Techniques for Accurate Diagnosis
1. Clinical History: This is the starting point for the diagnostic process. The ophthalmologist will gather details about the onset, duration, and progression of visual symptoms. Information about underlying systemic diseases, medications, and previous ocular surgeries can also offer crucial clues.
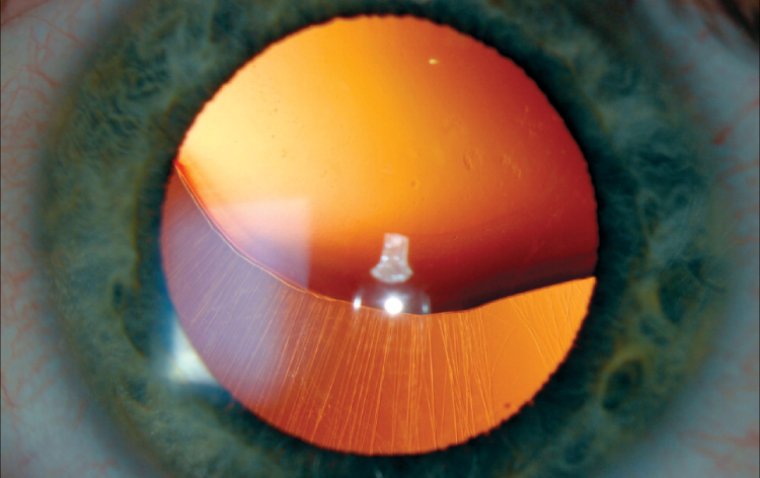
2. Ophthalmoscopic Examination: Through a dilated pupil, the ophthalmologist will inspect the optic nerve head. In acute ION, swelling or edema of the optic disc might be observed. In chronic or old cases, the optic disc may appear pale or atrophic.
3. Visual Acuity and Field Testing: A decrease in visual acuity and specific visual field defects, like an altitudinal defect, can support the diagnosis of ION. Automated perimetry, a visual field assessment, helps map out the exact areas of vision loss.
The Importance of Imaging Tests, Visual Field Assessments, and Blood Tests
● Optical Coherence Tomography (OCT): This non-invasive imaging test provides cross-sectional images of the retina, helping to assess the optic nerve and surrounding retinal nerve fiber layer. Edema or thinning can be detected in ION cases.
● Fluorescein Angiography: This imaging technique visualizes the circulation in the retina and choroid, potentially identifying areas of poor blood flow that could be contributing to the ION.
● Blood Tests: Especially relevant for arteritic ION (AION), blood tests like Erythrocyte Sedimentation Rate (ESR) and C-reactive protein (CRP) can indicate inflammation. Temporal artery biopsy might be recommended in cases suspected of giant cell arteritis.
Differential Diagnosis to Rule Out Other Causes of Optic Nerve Damage
Several other conditions can mimic the symptoms and signs of ION. Therefore, differential diagnosis is crucial. Conditions to rule out include:
1. Optic Neuritis: Often associated with multiple sclerosis, it presents with pain on eye movement and a different pattern of vision loss.
2. Compressive Optic Neuropathy: Tumors or lesions pressing on the optic nerve can cause vision changes.
3. Glaucomatous Optic Neuropathy: Linked with elevated intraocular pressure, it usually has a more gradual onset and a distinctive optic disc appearance.
4. Hereditary and Toxic Optic Neuropathies: These can result from genetic factors or exposure to certain medications or toxins.
Ischemic Optic Neuropathy Treatment
Ischemic Optic Neuropathy (ION) remains a challenging condition to manage. Treatment options largely depend on the type (arteritic or non-arteritic) and underlying causes. While some interventions aim to restore vision, others are focused on preventing further visual decline or managing the root causes.
Non-Surgical Approaches: Lifestyle Changes and Medications
1. Lifestyle Changes: For those with risk factors such as hypertension, diabetes, or high cholesterol, maintaining proper control over these conditions is imperative. Adopting a heart-healthy lifestyle with regular exercise, a balanced diet, and avoiding tobacco can potentially lower the risk of further ischemic events.
2. Medications:
● Blood Pressure Management: Antihypertensive medications may be prescribed to keep blood pressure at optimal levels.
● Blood Thinners: In some cases, antiplatelet or anticoagulant medications like aspirin might be recommended to reduce the risk of clot formation and further vascular events.
● Cholesterol Control: Statins or other lipid-lowering medications can be beneficial if dyslipidemia is identified as a risk factor.
Role of Corticosteroids and Anti-inflammatory Drugs in Reducing Inflammation
For arteritic ION, which is commonly associated with giant cell arteritis (GCA), inflammation of the blood vessels is a primary concern. Here's where corticosteroids come into play:
● High-dose Corticosteroids: These are the first line of treatment for GCA and can help reduce inflammation quickly. Immediate treatment is vital to prevent vision loss in the other eye.
● Long-term Steroid Use: While steroids are effective, their long-term use can come with side effects. Under a physician's guidance, the dosage is typically tapered over time, balancing the benefits and potential risks.
Surgical Interventions in Severe Cases and Potential Risks Involved
While the primary management of ION is medical, surgical options have been explored, especially for non-arteritic ION.
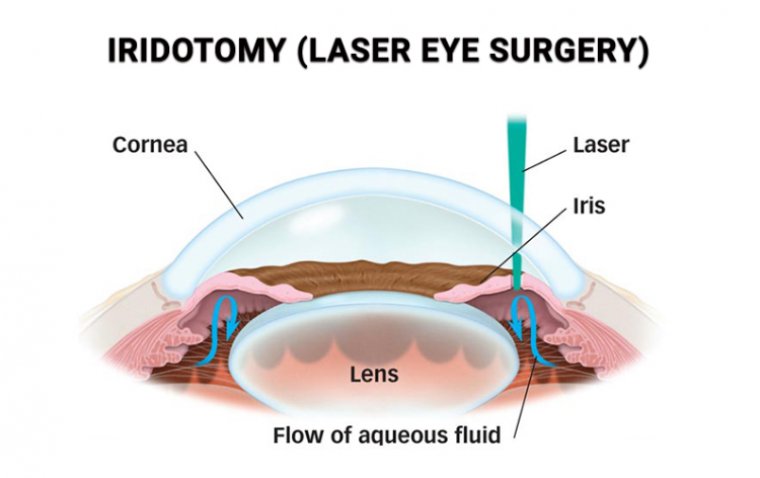
1. Optic Nerve Sheath Decompression: This procedure involves making small incisions in the lining around the optic nerve, aiming to relieve pressure and improve blood flow. However, its efficacy remains controversial, and it's not widely accepted.
2. Risks Involved: As with any surgical procedure, there are inherent risks, such as infection, bleeding, or further vision loss. It's essential to weigh the potential benefits against the risks.
Prognosis Based on the Type and Severity of the Condition
1. Arteritic ION: Typically associated with giant cell arteritis, this form often has a poorer prognosis. Immediate treatment with corticosteroids can prevent further vision loss, especially in the unaffected eye, but the vision already lost is often irreversible.
2. Non-Arteritic ION: The prognosis is somewhat better. Some patients may experience partial spontaneous visual improvement, usually within the first few weeks. However, complete recovery is rare.
3. Severity Factor: The extent of vision loss at the time of diagnosis can influence the prognosis. Earlier detection and intervention often correlate with better outcomes.
Summary
Ischemic Optic Neuropathy is a condition characterized by disrupted blood flow to the optic nerve, leading to potential vision loss. Various factors can lead to ION. Notably, arteritic and non-arteritic causes are the most common. Other risks include aging, cardiovascular conditions, systemic diseases, and certain lifestyle factors. Symptoms often involve visual disturbances, either appearing suddenly or gradually over time.
Diagnosis typically comprises comprehensive eye examinations, imaging tests like MRI or CT scans, visual field assessments, and blood tests. Treatment largely depends on the cause and severity, ranging from medications like corticosteroids to surgical interventions in more severe cases.
For prevention, maintaining cardiovascular health, frequent medical check-ups, and regular eye exams are pivotal. The prognosis of ION varies based on its type and severity. Still, regular follow-ups can help manage the condition effectively and detect any complications early on. It's imperative for individuals to be proactive in their eye care, especially when dealing with conditions that might lead to ION.