Yamane Technique: Sutureless Intrascleral IOL Fixation Explained
In cataract surgery, the optimal outcome involves implanting an intraocular lens (IOL) within the capsular bag. However, complications such as posterior capsule rupture, congenital lens anomalies, or traumatic injuries can leave patients without adequate capsular support, resulting in aphakia—a condition where the eye lacks a natural lens. Managing aphakia without capsular support requires alternative IOL fixation techniques to restore vision effectively.
Challenges in Cataract Surgery: Aphakia Without Capsular Support
Aphakia presents significant visual impairment and challenges in lens implantation. Traditional methods may not be suitable due to the absence of the capsular bag, necessitating innovative solutions to securely fixate the IOL in the correct anatomical position.
Overview of Scleral Fixation Techniques
Several surgical approaches address the lack of capsular support:
• Anterior Chamber IOLs (AC-IOLs): Placed in front of the iris but associated with risks like corneal endothelial damage and glaucoma.
• Iris-Claw IOLs: Attached to the iris but not ideal in cases with iris defects.
• Scleral-Fixated IOLs (SF-IOLs): Positioned posterior to the iris, offering long-term stability and a location similar to the natural lens.
Among these, SF-IOLs are favored for their stability and reduced risk of corneal complications.
The Yamane Technique Explained
What Is the Yamane Technique?
Introduced by Dr. Shin Yamane, the Yamane technique is a sutureless method for intrascleral IOL fixation, ideal for patients without capsular support. It involves creating scleral tunnels and using the IOL's haptics (supporting arms) to secure the lens in place.
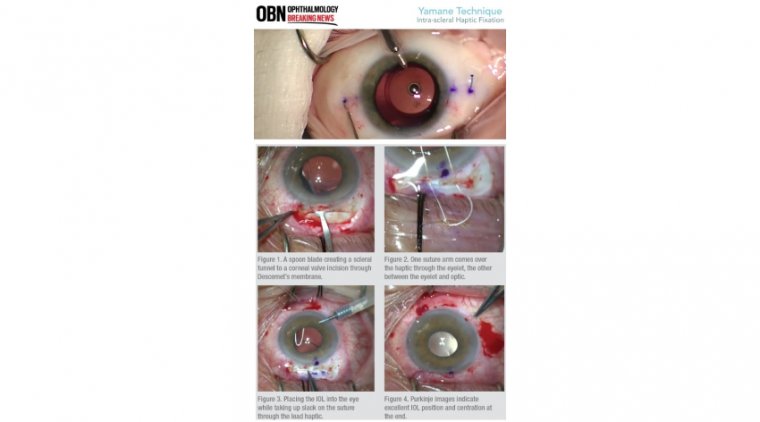
Step-by-Step Procedure
- Insertion of a Three-Piece IOL: A foldable, three-piece IOL is inserted into the anterior chamber of the eye.
- Creating Scleral Tunnels: Two 30-gauge thin-walled needles create scleral tunnels approximately 2.5 mm behind the limbus (the border between the cornea and sclera) at opposite sides.
- Externalizing the Haptics: The haptics are threaded into the needles and externalized through the scleral tunnels.
- Forming Flanges: The external ends of the haptics are cauterized to form small flanges.
- Securing the IOL: The flanged ends are tucked back into the scleral tunnels, anchoring the IOL without sutures.
Advantages of the Yamane Technique
• Sutureless Fixation: Eliminates suture-related complications.
• Reduced Surgical Time: Streamlined procedure compared to traditional methods.
• Stable IOL Positioning: Minimizes the risk of lens dislocation and tilt.
• Anatomical Placement: Positions the IOL in the posterior chamber, closely mimicking the natural lens location.
Clinical Cases Utilizing the Yamane Technique
Case 1: Dislocated IOL Due to Posterior Capsule Tear
A patient experienced an IOL dislocation after a posterior capsule tear during cataract surgery. The IOL obstructed the visual axis, causing poor vision. Using the Yamane technique:
• The dislocated IOL was safely removed.
• A new three-piece IOL was implanted and fixated using intrascleral haptic fixation.
• The patient's visual function was restored with proper lens positioning.
Case 2: Aphakia with Iris Defect Post-Vitrectomy
Another patient presented with:
• Aphakia due to lens removal during vitrectomy.
• An iris defect from a sector iridectomy.
• No capsular support for traditional IOL implantation.
The Yamane technique allowed for:
• Scleral fixation of a new IOL despite the lack of capsular and iris support.
• Concurrent iris repair to address the defect.
• Successful restoration of visual acuity and eye anatomy.
Key Surgical Considerations and Learning Points
Precision in Measurements and Markings
• Accurate Placement: Mark scleral entry points 2.5 mm posterior to the limbus and 180 degrees apart.
• Avoiding Decentration: Inconsistent measurements can lead to lens tilt or displacement.
Enhancing Visibility
• Conjunctival Opening: Improves visualization of scleral landmarks for precise needle insertion.
• Avoiding Globe Rotation: Stabilize the eye during needle passage to maintain alignment.
Needle Handling and Globe Stabilization
• Ambidexterity Required: Surgeons must use both hands effectively for symmetrical needle placement.
• Needle Angling: Proper angulation ensures correct scleral tunnel creation.
Threading the Haptics
• Micro-Instrumentation: Use fine instruments like 23-gauge micro-graspers for precise manipulation.
• Needle Alignment: Align the needle towards the haptic rather than moving the haptic excessively.
Equipment and IOL Selection for the Yamane Technique
Intraocular Lens Choice
• Three-Piece IOLs: Preferably with polyvinylidene fluoride (PVDF) haptics for flexibility and durability.
• Examples: CT Lucia 602 lens is commonly used due to its suitable haptic properties.
Surgical Instruments
• 30-Gauge Thin-Walled Needles: Essential for creating scleral tunnels and externalizing haptics.
• Low-Temperature Cautery: Used to form flanges on the haptic ends.
• Anterior Chamber Maintainer: Helps maintain intraocular pressure during the procedure.
Conclusion: Mastering the Yamane Technique
The Yamane technique offers an effective solution for patients with aphakia without capsular support. While there is a learning curve, especially regarding ambidextrous needle handling and precise measurements, surgeons can achieve excellent outcomes with practice and preparation. Proper equipment selection and adherence to the technique's principles are crucial for success.
By adopting the Yamane technique, ophthalmic surgeons can expand their surgical repertoire, offering patients improved visual outcomes in complex cases where traditional IOL implantation is not feasible.
References:
-
Yamane, S., Inoue, M., Arakawa, A., & Kadonosono, K. (2014). Flanged Intrascleral Intraocular Lens Fixation with Double-Needle Technique. Ophthalmology, 121(1), 61-66.
-
Kelkar, A., Kelkar, J., Mehta, H., & Amoaku, W. (2017). Sutureless 27-gauge Needle-guided Intrascleral IOL Fixation: Yamane Technique. Indian Journal of Ophthalmology, 65(12), 1449-1452.
-
Szurman, P., Petermeier, K., Aisenbrey, S., & Spitzer, M. S. (2010). Sutureless Intrascleral Posterior Chamber Lens Fixation. Journal of Cataract & Refractive Surgery, 36(11), 2080-2082.
-
Ohta, T., Toshida, H., Matsui, A., Honda, R., & Oki, K. (2019). Clinical Outcomes of Flanged Intrascleral Intraocular Lens Fixation Using Double-Needle Technique. Clinical Ophthalmology, 13, 2889-2894. Link
-
American Academy of Ophthalmology. (2019). Intrascleral Fixation Techniques for Secondary IOL Placement. Retrieved from AAO EyeWiki
(1).jpg)