Study Identifies Metabolic Stress as a Major Barrier to Retinal Cell Transplant Survival
Cell replacement therapy is emerging as a promising avenue for treating retinal degenerations (RDs), a group of sight-threatening disorders caused by the progressive loss of light-sensing photoreceptor cells. Among the leading experimental strategies is the transplantation of stem cell-derived photoreceptor precursor cells. These partially differentiated cells are intended to replace degenerated photoreceptors and potentially restore visual function. However, a major challenge persists: many of the transplanted cells fail to survive in the subretinal environment, hindering therapeutic success.
Investigating Early Cell Death Post-Transplantation
A research team from the Division of Experimental Retinal Therapies (ExpeRTs) at the University of Pennsylvania School of Veterinary Medicine, led by Raghavi Sudharsan and William A. Beltran, in collaboration with the University of Wisconsin–Madison and Harvard Medical School, has uncovered a key cause behind early donor cell loss.
In findings published in Stem Cell Research & Therapy, the researchers demonstrate that a significant portion of photoreceptor precursor cells undergo cell death within the first few days of transplantation into the subretinal space. This occurs even when immune rejection is effectively managed. The underlying cause was identified as acute metabolic stress, resulting from the abrupt transition between the nutrient-rich in vitro culture environment and the relatively nutrient-limited subretinal space.
Metabolic Stress: An Overlooked Threat
“This study highlights how vulnerable transplanted cells are during the initial days post-injection,” stated Dr. Sudharsan, assistant professor of experimental ophthalmology. “While immune rejection has been a longstanding focus, our results emphasize that metabolic stress must also be addressed for these therapies to succeed.”
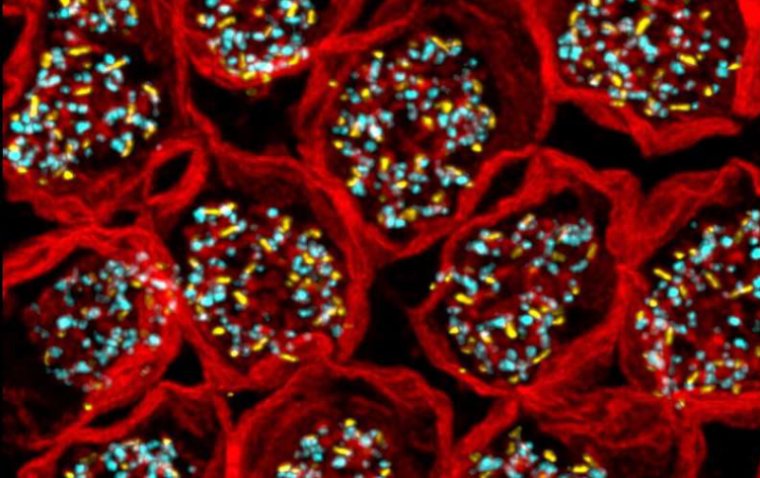
The research utilized noninvasive imaging techniques and single-cell RNA sequencing to analyze the transplanted cells. The data revealed strong signatures of oxidative damage and acute metabolic stress. These findings were further validated through immunohistochemistry, confirming the onset of cell death shortly after transplantation.
Optimizing the Therapeutic Window
Despite the widespread early cell loss, a subset of donor cells demonstrated the ability to survive and mature post-transplantation. In retinal models where some native photoreceptors remained intact, these surviving cells even initiated the formation of synapse-like structures, suggesting partial integration into the host retinal network.
Timing emerged as a critical variable. In models with partially intact photoreceptor layers, transplanted cells successfully integrated. Conversely, in end-stage degeneration models where retinal architecture was severely compromised, donor cell survival was not sustained.
“Some level of native photoreceptor loss appears necessary to enable donor cell integration,” said Dr. Beltran, Corinne R. and Henry Bower Professor of Ophthalmology and Director of ExpeRTs. “However, if degeneration advances too far, the environment becomes too hostile to support transplanted cells.”
Strategic Implications for Retinal Cell Therapy
The findings underscore the importance of defining a therapeutic window, where retinal damage is sufficient to permit integration but not extensive enough to prevent cell survival. The study suggests that optimizing the timing of transplantation and introducing supportive strategies could significantly improve therapeutic outcomes.
Potential interventions to mitigate early metabolic stress include preconditioning donor cells, using scaffold-based delivery systems, or supplementing nutrients during transplantation.
“As we move closer to clinical translation,” Dr. Sudharsan concluded, “a deep understanding of both donor cell biology and host retinal response will be crucial for designing effective, durable cell replacement therapies.”
Reference:
Raghavi Sudharsan et al, Metabolic stress and early cell death in photoreceptor precursor cells following retinal transplantation, Stem Cell Research & Therapy (2025). DOI: 10.1186/s13287-025-04509-w
(1).jpg)