Stanford Study Identifies New Method for Measuring Choroidal Tumor Thickness
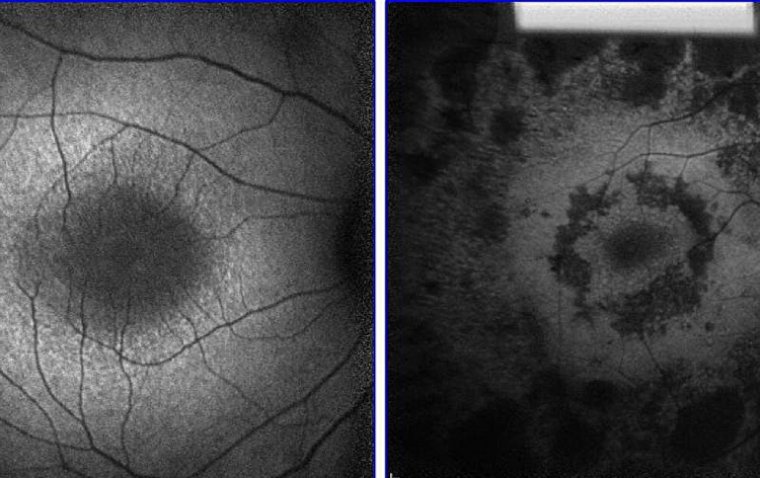
Researchers from the Ocular Oncology Service at the Byers Eye Institute and the Department of Radiation Oncology at Stanford University have proposed a novel technique for estimating choroidal tumor thickness using ultra-widefield (UWF) green-channel (GC) imaging. This non-invasive method could potentially eliminate the need for B-scan ultrasonography, which is not always readily available in clinical settings.
The Importance of Tumor Thickness in Choroidal Melanoma
Tumor thickness is a critical risk factor for the malignant transformation of choroidal nevi into melanoma. Traditionally, B-scan ultrasonography has been the gold standard for measuring choroidal tumor thickness. However, the Stanford study presents an innovative alternative using Optomap UWF GC imaging.
According to Michael D. Yu, MD, the study demonstrates a strong correlation between tumor thickness and pixel intensity differences (PID) on UWF GC images, suggesting that tumor thickness can be accurately estimated without relying on ultrasound imaging.
Study Design and Methodology
The researchers conducted a retrospective, cross-sectional study involving 138 patients with melanocytic choroidal lesions:
• 125 patients with choroidal nevi
• 13 patients with choroidal melanoma
The study aimed to:
• Correlate tumor thickness measurements from B-scan ultrasonography with the PID values from UWF GC images.
• Evaluate the sensitivity and specificity of the regression analysis trendline in estimating tumor thickness.
Key Findings: Correlation Between PID and Tumor Thickness
The results revealed a strong correlation between PID and tumor thickness:
• Mean ultrasonographic tumor thickness: 1.1 mm (median: 0.8 mm; range: 0.2–5.5 mm)
• Mean PID: 2.13
When the lesions were stratified by thickness:
• Tumors <1.0 mm: Mean PID -1.95; Mean thickness 0.5 mm
• Tumors 1.0–2.0 mm: Mean PID 3.72; Mean thickness 1.4 mm
• Tumors >2.0 mm: Mean PID 17.62; Mean thickness 3.3 mm
The researchers observed a statistically significant correlation (R² = 0.823; 95% CI, 0.770–0.875; P < .001) across lesions of all sizes.
Clinical Implications and Future Potential
The study suggests that UWF Optomap GC imaging could serve as a reliable, accessible, and rapid tool for measuring choroidal tumor thickness, especially in clinical settings where B-scan ultrasonography may not be available.
Dr. Yu and his team concluded that this method:
• Enhances diagnostic efficiency by eliminating the need for specialized ultrasound equipment.
• Improves accessibility to choroidal tumor monitoring in resource-limited settings.
• Supports earlier detection and monitoring of tumor growth in patients with choroidal nevi at risk for malignant transformation.
Conclusion: A Step Forward in Ocular Oncology
The Stanford study highlights the potential of Optomap UWF GC imaging as a non-invasive, efficient alternative to B-scan ultrasonography for measuring choroidal tumor thickness. By providing clinically relevant tumor measurements with a high degree of accuracy, this method could become a valuable tool for ocular oncology specialists and improve the management of patients with choroidal tumors.
Reference:
Yu MD, Heiferman M, Korot E, et al. Pixel intensity to estimate choroidal tumor thickness using 2-dimensional ultra-widefield images. JAMA Ophthalmol. JAMA Ophthalmol. 2025;Published online February 6; doi:10.1001/jamaophthalmol.2024.6064
(1).jpg)