Microdrops Show Potential for Safer Retinopathy of Prematurity Screening in Preterm Infants
A groundbreaking study by Greek researchers has demonstrated that microdrops containing 1.67% phenylephrine and 0.33% tropicamide are not only effective but also safer alternatives to standard mydriatic eye drops used during retinopathy of prematurity (ROP) screenings in preterm infants.
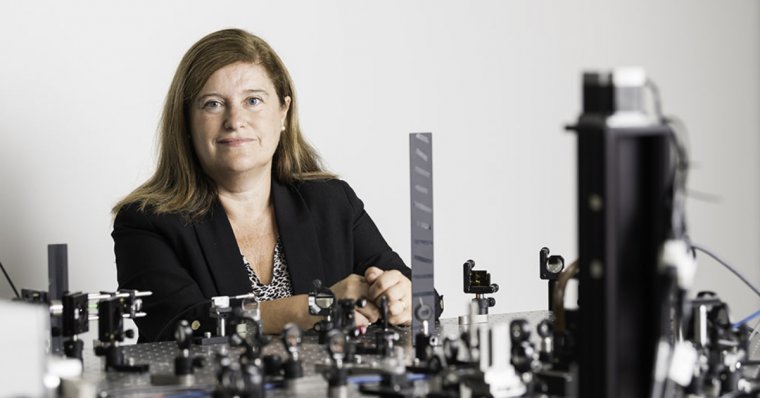
Led by Aikaterini K. Seliniotaki, MD, MSc, PhD, from the Second Department of Ophthalmology and the Department of Hygiene, Social-Preventive Medicine & Medical Statistics at Aristotle University of Thessaloniki, the study aimed to address the systemic adverse effects associated with traditional mydriatic drops.
Study Design: MyMiROPS Clinical Trial
The research, part of the MyMiROPS Randomized Clinical Trial (ClinicalTrials.gov Identifier: NCT05043077), was conducted at a tertiary center in Northern Greece between September 2021 and January 2023.
Rationale
Commercial mydriatic drops used during ROP screening are linked to cardiorespiratory and gastrointestinal adverse events, prompting the need for a safer alternative.
Objectives
The study aimed to assess whether the microdrops were:
1. Noninferior to standard drops in terms of mydriatic efficacy at 45, 90, and 120 minutes.
2. Safer, with reduced systemic adverse events.
Participants
• 83 preterm infants (mean gestational age: 29.7 weeks; mean birth weight: 1,277 grams).
• All participants had a gestational age below 32 weeks and/or a birth weight under 1,501 grams.
Methods
• Measurements:
- Horizontal pupil diameters were assessed at 45, 90, and 120 minutes.
- Heart rate, oxygen saturation, and blood pressure were recorded at the same intervals.
- 24-hour hypertensive episodes and 48-hour systemic adverse events were evaluated.
- Phenylephrine concentration in peripheral blood was measured within 3 hours post-instillation.
• Noninferiority Margin: Defined as −0.4 mm.
Key Outcomes
Efficacy
The microdrops were:
• Superior in mydriatic efficacy at 45 minutes (mean difference: 0.12 mm; Bonferroni-corrected 95% CI: 0.01-0.23; P = 0.008).
• Noninferior at 90 minutes (Bonferroni-corrected 95% CI: −0.10-0.17) and 120 minutes (Bonferroni-corrected 95% CI: −0.18-0.14).
Safety
• Standard drops resulted in:
- Lower oxygen saturation at 45 minutes (mean difference: 0.66; 95% CI: 0.09-1.24; P = 0.03) and 90 minutes (mean difference: 0.58; 95% CI: 0.03-1.14; P = 0.04).
- Higher percentage of 24-hour hypertensive episodes (0.14% [0.06%-0.40%]; P = 0.01) compared to microdrops (median: 0.10% [0.02%-0.19%]).
Conclusion
Dr. Seliniotaki and colleagues concluded:
“To our knowledge, this is the first study establishing the noninferiority of microdrops compared with standard drops of a diluted mydriatic mixture, showing reduced systemic adverse events after microdrops and determining the pharmacokinetic profile of phenylephrine eye drops in preterm infants.”
Implications
The findings suggest that microdrops could be a safer and equally effective alternative for ROP screenings, potentially improving outcomes for preterm infants while minimizing systemic risks. This represents a significant step forward in neonatal ophthalmic care.
Reference:
Seliniotaki AK, Lithoxopoulou M, Virgiliou C, et al. Retinopathy of prematurity screening. The MyMiROPS Randomized Clinical Trial. JAMA Ophthalmology doi:10.1001/jamaophthalmol.2024.5462
(1).jpg)