Novel AI Detects Retinopathy of Prematurity with 100% Accuracy
In a study published in JAMA Ophthalmology, researchers from Oregon Health & Science University (OHSU) alongside international collaborators have unveiled an artificial intelligence (AI) technology capable of independently detecting all severe cases of a condition leading to blindness in prematurely born infants.
Understanding Retinopathy of Prematurity (ROP)
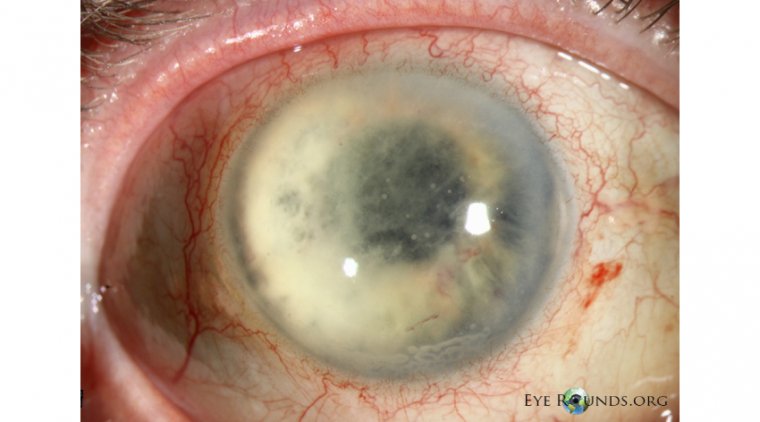
This condition, known as retinopathy of prematurity (ROP), is responsible for blindness in individuals such as the renowned musician Stevie Wonder. ROP is characterized by abnormal growth of blood vessels near the retina, the light-sensitive layer at the back of the eye. Annually, around 2 million babies are born prematurely, placing them at risk of ROP, which, in severe cases, leads to blindness in about 500 babies in the United States and approximately 50,000 worldwide. The disparity in treatment accessibility is more pronounced in low- and middle-income countries, where a shortage of ophthalmologists exacerbates the situation.
The Role of AI in Combatting ROP
"ROP is the leading cause of blindness in children in the U.S. and globally, representing a significant yet largely preventable challenge in the fight against blindness," stated J. Peter Campbell, M.D., M.P.H., the study's corresponding author and an associate professor of ophthalmology at the OHSU School of Medicine and OHSU Casey Eye Institute. He emphasized the critical shortage of doctors skilled in ROP treatment worldwide, highlighting the potential of AI to fill this gap by conducting bedside screenings and referring urgent cases for treatment.
i-ROP Deep Learning System
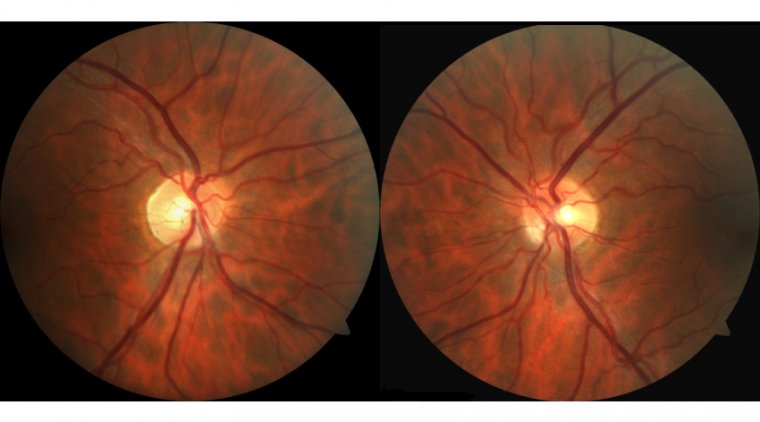
The technology at the heart of this innovation is the i-ROP Deep Learning system, developed by Michael Chiang, M.D., and his team while at OHSU, now the director of the National Eye Institute of the National Institutes of Health. Unlike traditional methods requiring manual analysis of retinal images by ophthalmologists, this AI algorithm autonomously identifies anomalies. Previous research demonstrated its accuracy in diagnosing ROP and its viability for remote use via telemedicine, expanding access to care.
This latest study marks the first successful real-world application of autonomous AI screening for ROP, analyzing nearly 12,000 images from over 4,000 infants' retinas taken in neonatal intensive care units across the U.S. and India. It impressively identified all severe ROP cases and accurately detected 80% of more-than-mild cases, showcasing its efficacy beyond controlled experimental settings where many AI algorithms falter due to discrepancies between training data and real-life applications.
Global Impact and Future Directions
Developed in collaboration with Massachusetts General Hospital, Northeastern University, University of Illinois Chicago, and the i-ROP consortium, the i-ROP Deep Learning system received breakthrough status from the Food and Drug Administration in 2020 to fast-track its development. Campbell, also the CEO of Siloam Vision which licensed the technology, is leading clinical trials to assess its safety and effectiveness. Moreover, through a partnership with Orbis International, the technology is being introduced in low- and middle-income countries, promising to mitigate the global burden of ROP.
If regulatory approvals are secured, ROP will become the second eye disease autonomously detectable by AI, following diabetic retinopathy. This marks a significant leap forward in using AI to enhance healthcare accessibility and effectiveness, particularly in underserved regions, and opens new avenues for preventing blindness in vulnerable populations worldwide.
Reference
Aaron S. Coyner et al, Multinational External Validation of Autonomous Retinopathy of Prematurity Screening, JAMA Ophthalmology (2024). DOI: 10.1001/jamaophthalmol.2024.0045
*Stay in the loop and make sure not to miss real-time breaking news about ophthalmology. Join our community by subscribing to OBN newsletter now, and get weekly updates.
(1).jpg)