Novel Stem Cell Therapy Repairs 'Irreversible' Corneal Damage in Clinical Trial
A phase I/II clinical trial evaluating an experimental stem cell therapy for corneal injuries has demonstrated feasibility, safety, and high success rates in restoring the corneal surface. The treatment, known as cultivated autologous limbal epithelial cells (CALEC), was developed at Mass Eye and Ear and has shown promising results in 14 patients over an 18-month follow-up period. The findings, published in Nature Communications, highlight the potential of stem cell therapy for previously untreatable corneal damage.
What is CALEC?
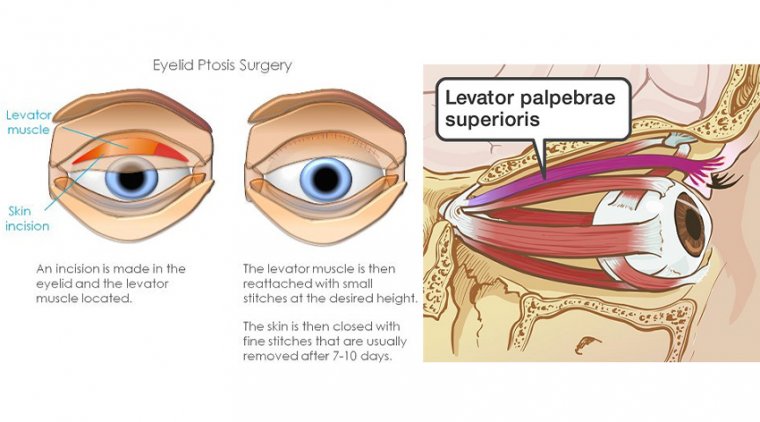
CALEC is a novel stem cell therapy designed to restore the cornea’s surface in patients with limbal stem cell deficiency caused by chemical burns, infections, or trauma. The procedure involves:
1. Extracting stem cells from a healthy eye using a small biopsy.
2. Expanding the cells into a cellular graft through a specialized manufacturing process over two to three weeks.
3. Transplanting the graft into the damaged cornea through surgery.
This approach addresses a critical limitation in corneal transplantation, where a damaged limbus prevents successful corneal grafting.
Clinical Trial Results
• At three months, CALEC fully restored the corneal surface in 50 percent of patients.
• By 12 and 18 months, the rate of complete success increased to 79 percent and 77 percent, respectively.
• Overall success, including partial improvements, reached 93 percent at 12 months and 92 percent at 18 months.
• Three patients required a second CALEC transplant, with one achieving full corneal restoration by the study’s end.
• All 14 patients showed various levels of improvement in visual acuity.
Safety and Tolerability
CALEC demonstrated a high safety profile, with no serious adverse events in either donor or recipient eyes. The only reported complication was a bacterial infection in one patient, eight months post-transplant, linked to chronic contact lens use. All other adverse events were minor and resolved quickly.
Current Status and Future Research
CALEC remains an experimental procedure and is not yet available at Mass Eye and Ear or any U.S. hospital. Further studies will be necessary before FDA approval can be pursued.
The research team, led by Ula Jurkunas, MD, along with Reza Dana, MD, Jia Yin, MD, PhD, and Myriam Armant, PhD, collaborated with the Dana-Farber Cancer Institute’s Connell and O’Reilly Families Cell Manipulation Core Facility and Boston Children’s Hospital to develop this therapy.
Expanding the Future of Stem Cell Therapy
CALEC relies on autologous transplantation, meaning it requires a healthy donor eye from the patient. Researchers are now exploring an allogeneic approach using limbal stem cells from cadaveric donors, which could:
• Expand the availability of the treatment to patients with bilateral corneal damage.
• Make the therapy accessible to a larger population.
“Our future hope is to establish an allogeneic manufacturing process, allowing patients with bilateral eye injuries to benefit from this therapy,” said Dr. Jerome Ritz of Dana-Farber Cancer Institute.
Next Steps Toward FDA Approval
The next phase of CALEC research will focus on:
• Larger, multi-center clinical trials.
• Longer follow-up periods to assess durability.
• Randomized-controlled studies for further validation.
“We believe this research warrants additional trials to advance towards FDA approval,” said Dr. Jurkunas. “Our ultimate goal is to ensure that patients across the country can access this life-changing therapy.”
With continued advancements in stem cell-based regenerative medicine, CALEC represents a breakthrough in corneal repair, offering hope for patients with previously irreversible eye injuries.
Reference:
Jurkunas, U et al. Cultivated autologous limbal epithelial cell (CALEC) transplantation for limbal tem cell deficiency: a phase I/II clinical trial of the first xenobiotic-free, serum-free, antibiotic-free manufacturing protocol developed in the US, Nature Communications (2025). DOI: 10.1038/s41467-025-56461-1
(1).jpg)