
New Guidelines By The European Glaucoma Society
New theories about the causes, processes, and treatments of glaucoma are constantly being developed. The European Glaucoma Society's mission is to advance the greatest level of health and the least amount of glaucoma-related visual impairment among glaucoma patients within an accessible healthcare system. The main problem was the advice for an initial treatment for open angle glaucoma and the function of the laser as primary therapy since the EGS modified recommendations for the initial open angle glaucoma treatment.
The European Glaucoma Society Committee used the GRADE process, which included the identification of key questions, critical evaluation of existing literature, and formulation of recommendations, to advance evidence-based therapeutic practice.
The Impact of the LiGHT Trial
Open angle glaucoma and ocular hypertension have long been successfully managed with laser trabeculoplasty. Betablockers, the top medicinal intervention at the time, were put up against argon laser trabeculoplasty in the historic US trial known as the Argon Laser Trabeculoplasty Trial (ALT). Despite the evidence in favor of ALT, medicines remained the go-to option for treating glaucoma.
The technical knowledge needed to implement ALT, the challenges of changing long-established practice, and cost considerations could all have contributed to this outcome (such as different reimbursement processes offered by healthcare providers and insurance companies). Whatever the reasons, ALT was never regarded as a first-line glaucoma treatment and still isn't. Even today, most people with recently discovered glaucoma begin taking medication. The LiGHT experiment, however, may be altering this.
Selective laser trabeculoplasty (SLT) has been the subject of numerous studies over the years, but until recently there has never been a significant, conclusive, high-quality study. Even if there is value in smaller studies, there is always a danger of generalizability and bias, which may be the reason why, despite evidence that laser therapy is equally as beneficial, drugs have remained the major course of treatment for glaucoma patients.
In the LiGHT experiment, it was discovered that SLT was both more efficient than eye drops in terms of controlling IOP, preventing the advancement of the condition, and reducing the need for glaucoma surgery. At the end of the three-year follow-up, 74% of the patients who had received SLT had no further need for eye drops. An worldwide leader (Gus Gazzard of Moorfields Eye Hospital in London, UK) oversaw the experiment, which had a patient population of more than 700 and low attrition rates.
These elements have had a substantial impact on the trial's favorable reputation. The trial's clear impact can be seen in the UK's National Institute for Health and Care Excellence (NICE) decision to revise their recommendations to recommend that lasers be used as a first-line treatment after its publication.
Lasers as First-Line Treatment
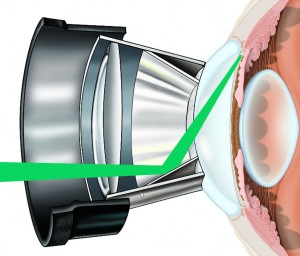
When it comes to drugs, patient compliance has always been a major problem. Increasing the number of glaucoma and ocular hypertension patients who receive laser therapy will, in our judgment, lead to better patient outcomes. Direct selective laser trabeculoplasty (DSLT), a cutting-edge laser procedure developed by BELKIN Laser Ltd., has the potential to completely transform the treatment of glaucoma. The technology is truly ground-breaking; providing the treatment only requires a few simple keystrokes and a few seconds of skill.
Importantly, general ophthalmologists will be able to provide laser trabeculoplasty even if they feel unqualified to provide ALT or SLT. This year will see the completion of a significant multicenter trial that compares SLT and DSLT. Additionally, the non-contact delivery method of DSLT makes it patient-friendly and eliminates the risk of infection, which is important to take into account in a post-pandemic environment.
That is not to say, however, that drugs won't continue to be crucial in the management of glaucoma. Since drugs are evolving as well, there are now more potent preservative-free eye drops available that lessen the usual adverse effects and tolerability problems.
(1).jpg)
Other New Considerations in the 2020 EGS Guidelines
The patient's voice was one essential, qualitative element we sought to offer with the new guidelines. However, this material was based on clinical opinion. In the previous 2016 edition of the EGS guidelines, we concentrated on the critical questions to ask patients as well as patients' potential concerns. In order to develop the new guidelines, we directly consulted with patients and patient representatives from a significant glaucoma charity (Glaucoma UK) about their top worries, most frequent anxieties, and other important issues to them, such as the most effective ways for surgeons to deliver the difficult news that a patient has glaucoma.
Even though this section is only a few pages long, it was crucial to include the patient's perspective in these recommendations. The fact that this version of the recommendations is evidence-based and uses quality control is another way it differs from earlier iterations.
As a result of our outreach efforts, the American Glaucoma Society, the World Glaucoma Association, and the Latin American Glaucoma Society were kind enough to provide feedback. They all gave excellent feedback, which also had an impact on some of the recommendations' content. This multi-national team effort marks a significant divergence from the earlier recommendations and supports the validity of those rules.
The Future
The guidelines have received largely positive feedback thus far. The impact of the rules, however, won't be known for some time because it takes time for people to consider the advice and alter their working habits. We are extremely confident in the effectiveness of the methodology employed, despite the fact that there is no such thing as a "perfect" set of standards. The management of glaucoma is currently in an exciting phase, with new alternatives emerging frequently and better therapies following closely behind. Yes, there are currently unmet demands in the treatment of glaucoma, but there is a great deal of room for advancement in the future.
(1).jpg)










